April 2020 Issue
ISSN 2689-291X
ISSN 2689-291X
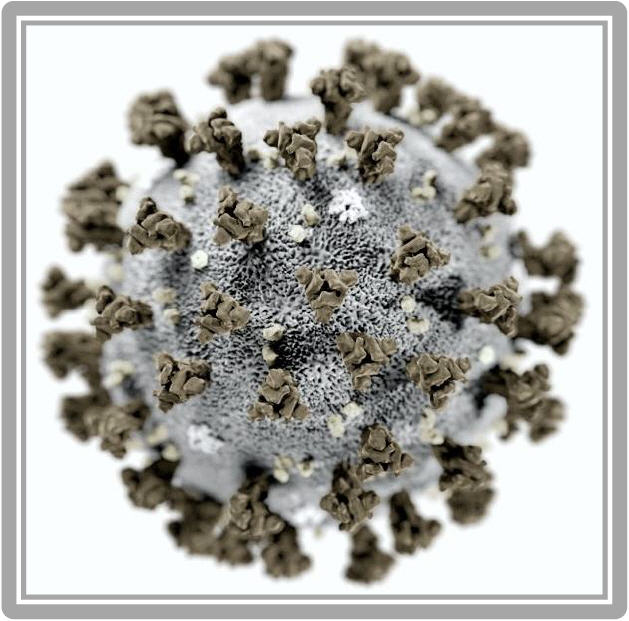
COronaVIrus Disease 2019 (COVID-19)
& The Cardiology Consultant
Introduction
The global COVID-19 pandemic caused by the novel coronavirus, SARS-CoV-2 is currently a worldwide public health crisis. Clinical presentations have varied from a mild respiratory viral syndrome to severe cases of acute respiratory failure and adult respiratory distress syndrome (ARDS), often accompanied by multisystem organ failure leading to death. The data available from around the world indicates that COVID-19 can have significant impact on the cardiovascular system and that pre-existing cardiac disease can influence how an infected patient responds to COVID-19. The following review is meant to highlight some of the data currently available and the role of the cardiology consultant in the care for COVID-19 infected patients.
Epidemiologic Characteristics and Cardiovascular Disease
A paper presented in China CDC Weekly by The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team provided the first insight into patient characteristics of those who were infected in China as of early February, 2020. They examined over 72,000 patient records, of which 44,672 patients were confirmed positive for COVID-19. The largest number of cases were documented in patients greater than 50 years of age. What was most alarming was that in the three age groups over 60 years of age (60-69, 70-79, and > 80) there was a significant increase in the number of deaths (30.2%, 30.5%, and 20.3%, respectively). These elderly patients carry multiple age-related comorbidities including various cardiac disease and cardiac risk factors. Patients in China who reported pre-existing cardiovascular disease (CVD), hypertension (HTN), or diabetes mellitus (DM) had some of the higher case fatality rates compared to those who had no comorbid conditions (10.5%, 6%, and 7.3%, respectively) [1]. In a smaller cohort of 138 hospitalized patients, there was greater need for ICU level care if they had preexisting CVD, HTN or DM [2]. Similarly, in a larger cohort of 1,099 patients, it was reported that such patients had a higher likelihood of intubation or death [3]. These patterns continue to hold true as the number of cases continues to climb. As of March 25, 2020 more than 430,000 patients in over 170 countries have been diagnosed with COVID-19, with the death toll approaching 20,000 [4].
Cardiologists and COVID-19 Patients
Initial Patient Care
It is clear from the data above that cardiologists will be on the front lines caring for COVID-19 or suspected COVID-19 patients. A recent article by Driggin et al. [5], listed few very salient points for the cardiologist to consider:
It is not surprising to see abnormal cardiac troponin values in this setting especially in the era of high sensitivity troponin assays. In fact, recent reports suggest that high sensitivity troponin levels were detectable in many patients with COVID-19 [2, 7-8]. Those patients with significant rise in troponin levels had a much worse prognosis overall [8]. A similar pattern holds true for natriuretic peptide levels. BNP and NT-proBNP levels, which are traditional markers of myocardial stress and/or heart failure, tend to be elevated in COVID-19 patients who present with significant respiratory symptoms, superimposed pneumonia, ARDS, or fulminant respiratory failure due to the secondary stress imposed on the myocardium. These values should be carefully interpreted with regards to the extent of cardiac involvement, in conjunction with other imaging studies such as chest radiography, chest computed tomography (CT) and echocardiography, especially point of care ultrasonography (POCUS) to decrease the risk of personnel and equipment exposure [9].
Mechanisms of Myocardial Injury
As the number of diagnosed cases of COVID-19 is increasing, it is becoming obvious that cardiovascular complications are an area of major concern. Elevated high sensitivity troponin I levels were reported in 12% of patients diagnosed with COVID-19 in one study [10]. Another smaller study of 138 patients [2] reported acute myocardial injury and cardiac rhythm disturbances in 7.2% and 16.7% of patients respectively. Patients with underlying CVD or cardiomyopathy are at highest risk for such cardiac complications. Troponin level elevation could reflect direct or indirect effects of the virus on the myocardium and cardiovascular system.
The mechanism of direct viral damage to the myocardium is thought to be related to angiotensin-converting enzyme 2 (ACE2). This membrane bound enzyme serves as the functional receptor via which the virus enters the cardiac myocyte. These receptors predominate in the heart and lung tissue. COVID-19 invades the alveolar epithelial cells which leads to significant respiratory symptoms. Direct invasion of myocardial cells could be a potential mechanism for acute myocardial injury, myocarditis, or other cardiac complications [7].
Indirect myocardial cell injury has also been demonstrated. The cytokine storm related to the viral infection and the body’s inflammatory system response, coupled with respiratory failure and hypoxemia, all add to the deleterious effects of the virus infection. Hypoxia caused by acute respiratory failure commonly seen with COVID-19 leads to widespread oxygen deprivation. Systemic inflammatory response can also lead to both type II, demand ischemia, myocardial injury (MI) as well as type I MI due to unstable coronary plaque rupture and increased hypercoagulability. Patients with underlying cardiomyopathy who develop acute illnesses find themselves battling acute heart failure exacerbations from multiple etiologies [7].
Consultative Recommendations
In addition to cardiology consultations often requested to assist in evaluating for acute coronary syndrome (ACS) or heart failure (HF) based on abnormal cardiac markers, as detailed earlier, few other critical issues have surfaced in relation to the care of COVID-19 patient, which would call for the cardiologist’s expertise.
One concern is regarding the use of renin-angiotensin-aldosterone system (RAAS) antagonists in patients with COVID-19 infection. Such medication, including angiotensin converting enzyme inhibitors (ACE-I), angiotensin receptor blockers (ARB), direct renin inhibitors, and aldosterone antagonists, are the mainstay treatment for patients with a wide variety of cardiovascular disease including hypertension, heart failure, and vascular disease. ACE2 receptors, as previously detailed, are the portal of entry for the coronavirus into the human body. The upregulation of ACE2 receptors by ACE inhibitors and ARBs has ignited a concern about the potential for increased risk of cardiac and pulmonary complications in COVID-19 patients on such medications. This concern was addressed by a joint statement [11] from the Heart Failure Society of America/American College of Cardiology and American Heart Association (HFSC/ACC/AHA). This statement, published March 17, 2020, mentions clearly that "there are no experimental or clinical data demonstrating beneficial or adverse outcomes among COVID-19 patients using ACE-I or ARB medications." The statement therefore urged clinicians to continue these medications in patients with HTN, HF, or ischemic heart disease, as long as they are tolerated, because of their well-established benefit. Ongoing research in this area should provide future insights into any potential clinical effect these agents may have on COVID-19 infected patients.
Another concern is the risk for COVID-19 exposure to health care workers and physicians when diagnostic studies and therapeutic interventions are needed. One statement released by the American College of Cardiology (ACC) and Society for Cardiovascular Angiography and Interventions (SCAI) addressed this concern in the catheterization lab [12] by calling for more conservative noninvasive treatment for Non-ST-segment Elevation Myocardial Infarction (NSTEMI) in COVID-19 pstients. The same statement urges consideration of thrombolysis in eligible ST-segment Elevation Myocardial Infarction (STEMI) patients who are COVID-19 positive or suspect rather than primary percutaneous coronary intervention (PCI). Cardiologists and other involved health care staff will likely need to bring their knowledge and skills up to date about thrombolysis, which has become nearly obsolete the past two decades, since the introduction of primary PCI as a more effective STEMI treatment. The statement further called for postponing all elective cardiac catheterization procedures to minimize potential exposure to patients and staff and to preserve the much needed protective personal equipment (PPE). Another recent statement from the American Society of Echocardiography (ASE) in response to the COVID-19 pandemic [13] stressed the importance of safety, minimizing the risk of exposure to healthcare providers, stating that “Use of UAPE (Ultrasound Assisted Physical Examination) and POCUS (Point Of Care Ultrasound) exams performed by the clinicians who are already caring for these patients at bedside presents an attractive option to screen for important cardiovascular findings, elucidate cardiac contributions to symptoms or signs, triage patients in need of full feature echocardiographic services and even, perhaps, identify early ventricular dysfunction during COVID-19 infection, all without exposing others and utilizing additional resources.”
A third concern is that the limited therapeutic options for COVID-19 patients has stirred interest in the potential role of hydroxychloroquine and azithromycin in treating the infection, which is currently under investigation. Both medications can prolong the QT interval, potentially causing serious ventricular arrhythmias. COVID-19 patients may also be prone to QT interval prolongation secondary to renal failure, hepatic failure, pre-existing cardiac disease, electrolyte abnormalities, and hypoxia, among other metabolic derangements. Patients treated with this combination of medications should undergo telemetry monitoring and scheduled electrocardiograms (ECGs) to measure the QT interval. Resources should be appropriated to allow for this to be accomplished under strict isolation measures to protect staff and allow for thorough sterilization of equipment after use [14].
A fourth issue concerns the potential use of ECMO (extracorporeal membrane oxygenation) in COVID-19 patients with ARDS who cannot maintain adequate oxygenation despite 100% FiO2 on mechanical ventilation. ECMO has traditionally been employed in prolonged cardiopulmonary failure, providing blood gas exchange for about 6 hours, bypassing the edematous lungs. The FDA has most recently, on April 7th 2020; issued guidance on this topic, stating that extracorporeal oxygenation can now be used for greater than six hours, recognizing the importance and utility of increased availability of ECMO devices for patients during the COVID-19 emergency, with further guidance on the various available devices [15]. This option obviously has limited availability and would require careful selection of patients for referral to tertiary centers where it can be offered.
Conclusion
The preceding account was not meant to be a comprehensive review of the cardiac complications of COVID-19, but rather to highlight a few key areas where the cardiologist’s expertise is needed. As this pandemic evolves and further information becomes available, cardiologists will most likely encounter new considerations they should be mindful of. It would be prudent to invoke a cardiology consultation early on when patients with known underlying cardiac disease are diagnosed with COVID-19 respiratory illness, given the severity and abruptness of potential cardiac complications and the risk of imminent death in this population. This deadly pandemic has strained health care resources in a way never before imaginable, calling for swift point of care innovations in the provision of care to extremely sick patients with novel ailments, when timely needed expert opinions can save lives. This is the time for the cardiology consultant to provide such expertise and recommendations, in collaborations with other consultants, to help their primary care and intensivist colleagues best achieve desirable outcomes and save lives through a more than ever needed multidisciplinary care approach.
References:
Authors:
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hassan Tahir, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
The global COVID-19 pandemic caused by the novel coronavirus, SARS-CoV-2 is currently a worldwide public health crisis. Clinical presentations have varied from a mild respiratory viral syndrome to severe cases of acute respiratory failure and adult respiratory distress syndrome (ARDS), often accompanied by multisystem organ failure leading to death. The data available from around the world indicates that COVID-19 can have significant impact on the cardiovascular system and that pre-existing cardiac disease can influence how an infected patient responds to COVID-19. The following review is meant to highlight some of the data currently available and the role of the cardiology consultant in the care for COVID-19 infected patients.
Epidemiologic Characteristics and Cardiovascular Disease
A paper presented in China CDC Weekly by The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team provided the first insight into patient characteristics of those who were infected in China as of early February, 2020. They examined over 72,000 patient records, of which 44,672 patients were confirmed positive for COVID-19. The largest number of cases were documented in patients greater than 50 years of age. What was most alarming was that in the three age groups over 60 years of age (60-69, 70-79, and > 80) there was a significant increase in the number of deaths (30.2%, 30.5%, and 20.3%, respectively). These elderly patients carry multiple age-related comorbidities including various cardiac disease and cardiac risk factors. Patients in China who reported pre-existing cardiovascular disease (CVD), hypertension (HTN), or diabetes mellitus (DM) had some of the higher case fatality rates compared to those who had no comorbid conditions (10.5%, 6%, and 7.3%, respectively) [1]. In a smaller cohort of 138 hospitalized patients, there was greater need for ICU level care if they had preexisting CVD, HTN or DM [2]. Similarly, in a larger cohort of 1,099 patients, it was reported that such patients had a higher likelihood of intubation or death [3]. These patterns continue to hold true as the number of cases continues to climb. As of March 25, 2020 more than 430,000 patients in over 170 countries have been diagnosed with COVID-19, with the death toll approaching 20,000 [4].
Cardiologists and COVID-19 Patients
Initial Patient Care
It is clear from the data above that cardiologists will be on the front lines caring for COVID-19 or suspected COVID-19 patients. A recent article by Driggin et al. [5], listed few very salient points for the cardiologist to consider:
- CVD specialists will actively be engaged in the care of COVID-19 patients.
- The infection may directly impact cardiovascular disease.
- Patients with preexisting CVD are at high risk for contracting COVID-19.
- Patients with preexisting CVD are at high risk for severe, life-threatening illness.
- Clinicians delivering cardiovascular care to the patients are at risk of infection themselves or serving as a vector for spread of the infection.
It is not surprising to see abnormal cardiac troponin values in this setting especially in the era of high sensitivity troponin assays. In fact, recent reports suggest that high sensitivity troponin levels were detectable in many patients with COVID-19 [2, 7-8]. Those patients with significant rise in troponin levels had a much worse prognosis overall [8]. A similar pattern holds true for natriuretic peptide levels. BNP and NT-proBNP levels, which are traditional markers of myocardial stress and/or heart failure, tend to be elevated in COVID-19 patients who present with significant respiratory symptoms, superimposed pneumonia, ARDS, or fulminant respiratory failure due to the secondary stress imposed on the myocardium. These values should be carefully interpreted with regards to the extent of cardiac involvement, in conjunction with other imaging studies such as chest radiography, chest computed tomography (CT) and echocardiography, especially point of care ultrasonography (POCUS) to decrease the risk of personnel and equipment exposure [9].
Mechanisms of Myocardial Injury
As the number of diagnosed cases of COVID-19 is increasing, it is becoming obvious that cardiovascular complications are an area of major concern. Elevated high sensitivity troponin I levels were reported in 12% of patients diagnosed with COVID-19 in one study [10]. Another smaller study of 138 patients [2] reported acute myocardial injury and cardiac rhythm disturbances in 7.2% and 16.7% of patients respectively. Patients with underlying CVD or cardiomyopathy are at highest risk for such cardiac complications. Troponin level elevation could reflect direct or indirect effects of the virus on the myocardium and cardiovascular system.
The mechanism of direct viral damage to the myocardium is thought to be related to angiotensin-converting enzyme 2 (ACE2). This membrane bound enzyme serves as the functional receptor via which the virus enters the cardiac myocyte. These receptors predominate in the heart and lung tissue. COVID-19 invades the alveolar epithelial cells which leads to significant respiratory symptoms. Direct invasion of myocardial cells could be a potential mechanism for acute myocardial injury, myocarditis, or other cardiac complications [7].
Indirect myocardial cell injury has also been demonstrated. The cytokine storm related to the viral infection and the body’s inflammatory system response, coupled with respiratory failure and hypoxemia, all add to the deleterious effects of the virus infection. Hypoxia caused by acute respiratory failure commonly seen with COVID-19 leads to widespread oxygen deprivation. Systemic inflammatory response can also lead to both type II, demand ischemia, myocardial injury (MI) as well as type I MI due to unstable coronary plaque rupture and increased hypercoagulability. Patients with underlying cardiomyopathy who develop acute illnesses find themselves battling acute heart failure exacerbations from multiple etiologies [7].
Consultative Recommendations
In addition to cardiology consultations often requested to assist in evaluating for acute coronary syndrome (ACS) or heart failure (HF) based on abnormal cardiac markers, as detailed earlier, few other critical issues have surfaced in relation to the care of COVID-19 patient, which would call for the cardiologist’s expertise.
One concern is regarding the use of renin-angiotensin-aldosterone system (RAAS) antagonists in patients with COVID-19 infection. Such medication, including angiotensin converting enzyme inhibitors (ACE-I), angiotensin receptor blockers (ARB), direct renin inhibitors, and aldosterone antagonists, are the mainstay treatment for patients with a wide variety of cardiovascular disease including hypertension, heart failure, and vascular disease. ACE2 receptors, as previously detailed, are the portal of entry for the coronavirus into the human body. The upregulation of ACE2 receptors by ACE inhibitors and ARBs has ignited a concern about the potential for increased risk of cardiac and pulmonary complications in COVID-19 patients on such medications. This concern was addressed by a joint statement [11] from the Heart Failure Society of America/American College of Cardiology and American Heart Association (HFSC/ACC/AHA). This statement, published March 17, 2020, mentions clearly that "there are no experimental or clinical data demonstrating beneficial or adverse outcomes among COVID-19 patients using ACE-I or ARB medications." The statement therefore urged clinicians to continue these medications in patients with HTN, HF, or ischemic heart disease, as long as they are tolerated, because of their well-established benefit. Ongoing research in this area should provide future insights into any potential clinical effect these agents may have on COVID-19 infected patients.
Another concern is the risk for COVID-19 exposure to health care workers and physicians when diagnostic studies and therapeutic interventions are needed. One statement released by the American College of Cardiology (ACC) and Society for Cardiovascular Angiography and Interventions (SCAI) addressed this concern in the catheterization lab [12] by calling for more conservative noninvasive treatment for Non-ST-segment Elevation Myocardial Infarction (NSTEMI) in COVID-19 pstients. The same statement urges consideration of thrombolysis in eligible ST-segment Elevation Myocardial Infarction (STEMI) patients who are COVID-19 positive or suspect rather than primary percutaneous coronary intervention (PCI). Cardiologists and other involved health care staff will likely need to bring their knowledge and skills up to date about thrombolysis, which has become nearly obsolete the past two decades, since the introduction of primary PCI as a more effective STEMI treatment. The statement further called for postponing all elective cardiac catheterization procedures to minimize potential exposure to patients and staff and to preserve the much needed protective personal equipment (PPE). Another recent statement from the American Society of Echocardiography (ASE) in response to the COVID-19 pandemic [13] stressed the importance of safety, minimizing the risk of exposure to healthcare providers, stating that “Use of UAPE (Ultrasound Assisted Physical Examination) and POCUS (Point Of Care Ultrasound) exams performed by the clinicians who are already caring for these patients at bedside presents an attractive option to screen for important cardiovascular findings, elucidate cardiac contributions to symptoms or signs, triage patients in need of full feature echocardiographic services and even, perhaps, identify early ventricular dysfunction during COVID-19 infection, all without exposing others and utilizing additional resources.”
A third concern is that the limited therapeutic options for COVID-19 patients has stirred interest in the potential role of hydroxychloroquine and azithromycin in treating the infection, which is currently under investigation. Both medications can prolong the QT interval, potentially causing serious ventricular arrhythmias. COVID-19 patients may also be prone to QT interval prolongation secondary to renal failure, hepatic failure, pre-existing cardiac disease, electrolyte abnormalities, and hypoxia, among other metabolic derangements. Patients treated with this combination of medications should undergo telemetry monitoring and scheduled electrocardiograms (ECGs) to measure the QT interval. Resources should be appropriated to allow for this to be accomplished under strict isolation measures to protect staff and allow for thorough sterilization of equipment after use [14].
A fourth issue concerns the potential use of ECMO (extracorporeal membrane oxygenation) in COVID-19 patients with ARDS who cannot maintain adequate oxygenation despite 100% FiO2 on mechanical ventilation. ECMO has traditionally been employed in prolonged cardiopulmonary failure, providing blood gas exchange for about 6 hours, bypassing the edematous lungs. The FDA has most recently, on April 7th 2020; issued guidance on this topic, stating that extracorporeal oxygenation can now be used for greater than six hours, recognizing the importance and utility of increased availability of ECMO devices for patients during the COVID-19 emergency, with further guidance on the various available devices [15]. This option obviously has limited availability and would require careful selection of patients for referral to tertiary centers where it can be offered.
Conclusion
The preceding account was not meant to be a comprehensive review of the cardiac complications of COVID-19, but rather to highlight a few key areas where the cardiologist’s expertise is needed. As this pandemic evolves and further information becomes available, cardiologists will most likely encounter new considerations they should be mindful of. It would be prudent to invoke a cardiology consultation early on when patients with known underlying cardiac disease are diagnosed with COVID-19 respiratory illness, given the severity and abruptness of potential cardiac complications and the risk of imminent death in this population. This deadly pandemic has strained health care resources in a way never before imaginable, calling for swift point of care innovations in the provision of care to extremely sick patients with novel ailments, when timely needed expert opinions can save lives. This is the time for the cardiology consultant to provide such expertise and recommendations, in collaborations with other consultants, to help their primary care and intensivist colleagues best achieve desirable outcomes and save lives through a more than ever needed multidisciplinary care approach.
References:
- Feng Z., Li Q, Zhang Y, et al. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Disease (COVID-19) - China, 2020. CCDC Weekly. February 14, 2020. Vol.2/No.8. 113-122.
- Wang D, Hu B, Hu C, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061-1069.
- Guan W, Ni Z, Hu Y, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. New Eng J Med. February 28, 2020. [epub ahead of print].
- Bonow RO, Fonarow GC, O’Gara PT, et al. Association of Coronavirus Disease 2019 (COVID-19) With Myocardial Injury and Mortality. JAMA Cardiol. Published online March 27, 2020.
- Driggin E, Madhavan MV, Bikdeli B, et al. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic. J Am Coll Cardiol. 2020 Mar 19.
- Coronavirus Disease 2019 (COVID-19) – Symptoms of Coronavirus. Https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html.
- Zheng YY, Ma YT, Zhang JY et al. COVID-19 and the cardiovascular system. Nat Rev Cardiol. March 5, 2020.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. March 11, 2020.
- James L. Januzzi Jr. Troponin and BNP Use in COVID-19. American College of Cardiology Magazine. https://www.acc.org/latest-in-cardiology/articles/2020/03/18/15/25/troponin-and-bnp-use-in-covid19.
- Huang C,Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395 (10223):497-506. doi:10.1016/S0140- 6736(20)30183-5.
- Bozkurt B, Kovacs R, Harrington R. HFSA/ACC/AHA Statement Addresses Concerns Re: Using RAAS Antagonists in COVID-19. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19. March 17, 2020.
- Welt FGP, Shah PB, Aronow HD, et al. Catheterization Laboratory Considerations During the Coronavirus (COVID-19) Pandemic: From ACC's Interventional Council and SCAI. J Am Coll Cardiol. 2020 Mar 16. pii: S0735-1097(20)34566-6.
- Kirkpatrick J, Mitchell C, Taub C, at al. ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak. https://www.asecho.org/ase-statement-covid-19/. Updated April 1 2020.
- Simpson T, Kovacs R, Stecker E. Ventricular Arrhythmia Risk Due to Hydroxychloroquine Azithromycin Treatment For COVID-19. https://www.acc.org/latest-in cardiology/articles/2020/03/ 27/14/00/ventricular-arrhythmia-risk-due-to-hydroxychloroquine-azithromycin-treatment-for-covid-19.
- Enforcement Policy for Extracorporeal Membrane Oxygenation and Cardiopulmonary Bypass Devices During the Coronavirus Disease 2019 (COVID-19) Public Health Emergency Guidance for Industry and Food and Drug Administration Staff April 2020. Https://www.fda.gov/media/136734/download
Authors:
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hassan Tahir, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL