April 2021 Issue
ISSN 2689-291X
ISSN 2689-291X
Tricuspid Valvulectomy..
Radical Cure for Recurrent Endocarditis!
Description
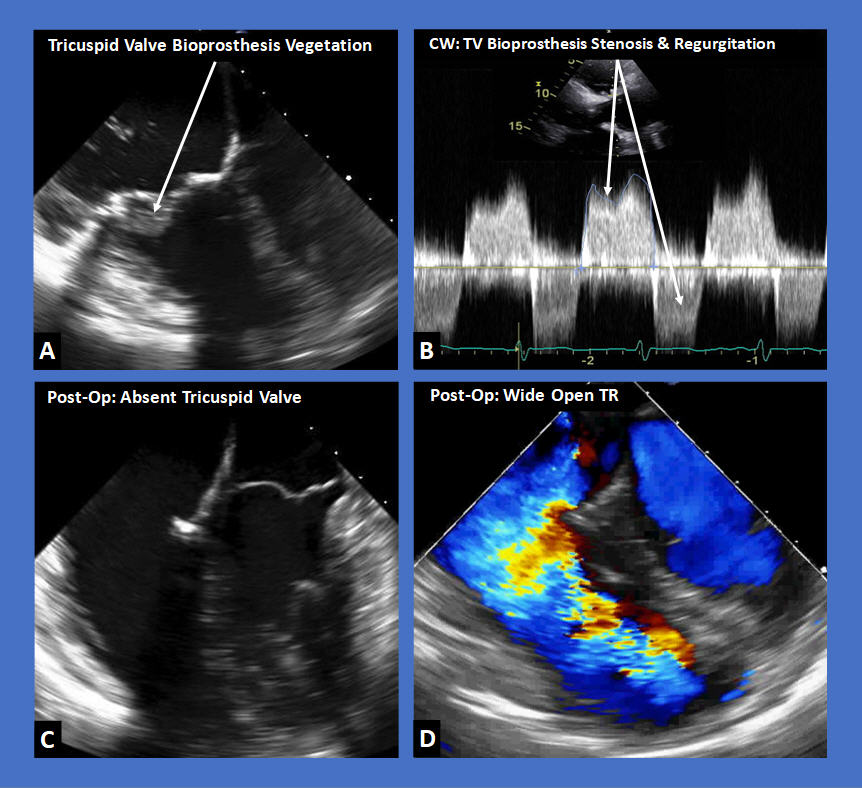
The figure above shows transesophageal echocardiographic images (TEE) of a tricuspid valve (TV) bioprosthesis with recurrent vegetation (Figure A). Continuous wave (CW) Doppler across the bioprosthesis in a 2-D modified parasternal echocardiographic view (Figure B) reveals both regurgitation and stenosis caused by the bulky vegetations. Figure C is a TEE image post-op TV bioprosthesis valvulectomy revealing absence of a valve in the tricuspid position, with resultant wide-open TR shown by color flow Doppler in Figure D.
Discussion
Infective endocarditis is a major health issue, affecting approximately 15 of 100,000 subjects, with a predilection to males and elderly, and continues to carry high mortality rates [1]. Right-sided endocarditis is less common than left sided endocarditis, and almost exclusively affects the tricuspid valve as a result of IV drug abuse, intracardiac implantable devices and dialysis vascular access. It is predominantly caused by Staphylococcus aureus [2].
Prosthetic valve endocarditis is less common, with a reported incidence of up to 1.2% per patient year, but can be detrimental, causing acute significant hemodynamic abnormalities and more often requires prompt surgical intervention [3]. Bioprosthetic valve endocarditis tends to be more common than mechanical valve endocarditis, likely due to leaflet degeneration and increased flow turbulence, lack of anticoagulation, compared with mechanical valves, and potentially lower utilization of SBE prophylaxis in bioprosthetic valves [4].
Medical and often surgical management are needed to treat endocarditis, especially of prosthetic valves, depending on the extent of valve damage and hemodynamic abnormalities [5]. While valve replacement is often required in left sided endocarditis due to the higher hemodynamic burden of valvular stenosis or regurgitation leading to heart failure, more options may be available in right sided endocarditis [6]. Tricuspid valve replacement is one option, although less ideal in the setting of intravenous drug abuse; bovine bioprostheses appear to have more long-term regurgitation [7]. Surgical tricuspid valve reconstruction, including vegectomy, debridement, and patch repair have also been reported [8]. Percutaneous vegectomy has been reported to result in significant debulking of tricuspid valve vegetations reducing embolic potential and reinfection rates [9]. These procedures mitigate the long term risk of severe tricuspid regurgitation associated with complete resection of the tricuspid valve (Valvulectomy).
Tricuspid valvulectomy without replacement, although represents an attractive option for intractable, recurrent tricuspid valve endocarditis, especially in IV drug abuse patients, is associated with severe tricuspid regurgitation and its attendant risks [10]. Right heart failure has been reported in 3 out of 10 patients undergoing tricuspid valvulectomy, with no definitive preop features to predict post-op outcomes [11]. Severe tricuspid regurgitation is associated with an overall increased long-term morbidity and mortality, calling for more intensive medical, surgical and interventional management [12]. The advent of catheter-based interventions, such as inferior vena cava percutaneous valve implantation, especially in high surgical-risk patients, has been demonstrated to ameliorate the hemodynamic effects of severe tricuspid regurgitation resulting in symptom improvement [13]. These interventions, however, await the support of larger clinical studies to establish a definitive role in improving outcomes in severe TR [14].
References:
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Lindsay Buono, M.D.
Surgery Resident
University of South Alabama
Mobile, AL
Jack Murfee, M.D.
Surgery Resident
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Carl Maltese, M.D.
Cardiovascular and Thoracic Surgeon
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The figure above shows transesophageal echocardiographic images (TEE) of a tricuspid valve (TV) bioprosthesis with recurrent vegetation (Figure A). Continuous wave (CW) Doppler across the bioprosthesis in a 2-D modified parasternal echocardiographic view (Figure B) reveals both regurgitation and stenosis caused by the bulky vegetations. Figure C is a TEE image post-op TV bioprosthesis valvulectomy revealing absence of a valve in the tricuspid position, with resultant wide-open TR shown by color flow Doppler in Figure D.
Discussion
Infective endocarditis is a major health issue, affecting approximately 15 of 100,000 subjects, with a predilection to males and elderly, and continues to carry high mortality rates [1]. Right-sided endocarditis is less common than left sided endocarditis, and almost exclusively affects the tricuspid valve as a result of IV drug abuse, intracardiac implantable devices and dialysis vascular access. It is predominantly caused by Staphylococcus aureus [2].
Prosthetic valve endocarditis is less common, with a reported incidence of up to 1.2% per patient year, but can be detrimental, causing acute significant hemodynamic abnormalities and more often requires prompt surgical intervention [3]. Bioprosthetic valve endocarditis tends to be more common than mechanical valve endocarditis, likely due to leaflet degeneration and increased flow turbulence, lack of anticoagulation, compared with mechanical valves, and potentially lower utilization of SBE prophylaxis in bioprosthetic valves [4].
Medical and often surgical management are needed to treat endocarditis, especially of prosthetic valves, depending on the extent of valve damage and hemodynamic abnormalities [5]. While valve replacement is often required in left sided endocarditis due to the higher hemodynamic burden of valvular stenosis or regurgitation leading to heart failure, more options may be available in right sided endocarditis [6]. Tricuspid valve replacement is one option, although less ideal in the setting of intravenous drug abuse; bovine bioprostheses appear to have more long-term regurgitation [7]. Surgical tricuspid valve reconstruction, including vegectomy, debridement, and patch repair have also been reported [8]. Percutaneous vegectomy has been reported to result in significant debulking of tricuspid valve vegetations reducing embolic potential and reinfection rates [9]. These procedures mitigate the long term risk of severe tricuspid regurgitation associated with complete resection of the tricuspid valve (Valvulectomy).
Tricuspid valvulectomy without replacement, although represents an attractive option for intractable, recurrent tricuspid valve endocarditis, especially in IV drug abuse patients, is associated with severe tricuspid regurgitation and its attendant risks [10]. Right heart failure has been reported in 3 out of 10 patients undergoing tricuspid valvulectomy, with no definitive preop features to predict post-op outcomes [11]. Severe tricuspid regurgitation is associated with an overall increased long-term morbidity and mortality, calling for more intensive medical, surgical and interventional management [12]. The advent of catheter-based interventions, such as inferior vena cava percutaneous valve implantation, especially in high surgical-risk patients, has been demonstrated to ameliorate the hemodynamic effects of severe tricuspid regurgitation resulting in symptom improvement [13]. These interventions, however, await the support of larger clinical studies to establish a definitive role in improving outcomes in severe TR [14].
References:
- Hubers SA, DeSimone DC, Gersh BJ, Anavekar NS. Infective Endocarditis: A Contemporary Review. Mayo Clin Proc. 2020 May;95(5):982-997.
- Hussain ST, Witten J, Shrestha NK, Blackstone EH, Pettersson GB. Tricuspid valve endocarditis. Ann Cardiothorac Surg. 2017 May;6(3):255-261.
- Mahesh B, Angelini G, Caputo M, Jin XY, Bryan A. Prosthetic valve endocarditis. Ann Thorac Surg. 2005 Sep;80(3):1151-8.
- Ya'qoub L, Eng MH. Bioprosthetic valve infective endocarditis: why is it important? Heart. 2020 Sep;106(18):1378-1379.
- Wang A, Gaca JG, Chu VH. Management Considerations in Infective Endocarditis: A Review. JAMA. 2018 Jul 3;320(1):72-83.
- Arbulu A, Holmes RJ, Asfaw I. Surgical treatment of intractable right-sided infective endocarditis in drug addicts: 25 years experience. J Heart Valve Dis. 1993 Mar;2(2):129-37.
- Wiedemann D, Rupprechter V, Mascherbauer J, Kammerlander A, Mora B, Dimitrov K, Weber B, Andreas M, Laufer G, Kocher A. Tricuspid valve replacement: results of an orphan procedure - which is the best prosthesis? J Cardiovasc Surg (Torino). 2018 Aug;59(4):626-632.
- Lange R, De Simone R, Bauernschmitt R, Tanzeem A, Schmidt C, Hagl S. Tricuspid valve reconstruction, a treatment option in acute endocarditis. Eur J Cardiothorac Surg. 1996;10(5):320-6.
- Thiagaraj AK, Malviya M, Htun WW, Telila T, Lerner SA, Elder MD, Schreiber TL. A novel approach in the management of right-sided endocarditis: percutaneous vegectomy using the AngioVac cannula. Future Cardiol. 2017 May;13(3):211-217.
- Arbulu A, Holmes RJ, Asfaw I. Tricuspid valvulectomy without replacement. Twenty years' experience. J Thorac Cardiovasc Surg. 1991 Dec;102(6):917-22.
- Robin E, Thomas NW, Arbulu A, Ganguly SN, Magnisalis K. Hemodynamic consequences of total removal of the tricuspid valve without prosthetic replacement. Am J Cardiol. 1975 Apr;35(4):481-6.
- Sadeghpour A, Hassanzadeh M, Kyavar M, Bakhshandeh H, Naderi N, Ghadrdoost B, Haghighat Talab A. Impact of severe tricuspid regurgitation on long term survival. Res Cardiovasc Med. 2013 Aug;2(3):121-6.
- Lauten A, Figulla HR, Unbehaun A, Fam N, Schofer J, Doenst T, Hausleiter J, Franz M, Jung C, Dreger H, Leistner D, Alushi B, Stundl A, Landmesser U, Falk V, Stangl K, Laule M. Interventional Treatment of Severe Tricuspid Regurgitation: Early Clinical Experience in a Multicenter, Observational, First-in-Man Study. Circ Cardiovasc Interv. 2018 Feb;11(2):e006061.
- Beckhoff F, Alushi B, Jung C, Navarese E, Franz M, Kretzschmar D, Wernly B, Lichtenauer M, Lauten A. Tricuspid Regurgitation - Medical Management and Evolving Interventional Concepts. Front Cardiovasc Med. 2018 May 28;5:49.
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Lindsay Buono, M.D.
Surgery Resident
University of South Alabama
Mobile, AL
Jack Murfee, M.D.
Surgery Resident
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Carl Maltese, M.D.
Cardiovascular and Thoracic Surgeon
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL