August 2021 Issue
ISSN 2689-291X
ISSN 2689-291X
Pacemaker Lead Mobile Mass..
Thrombus or Vegetation!
Description
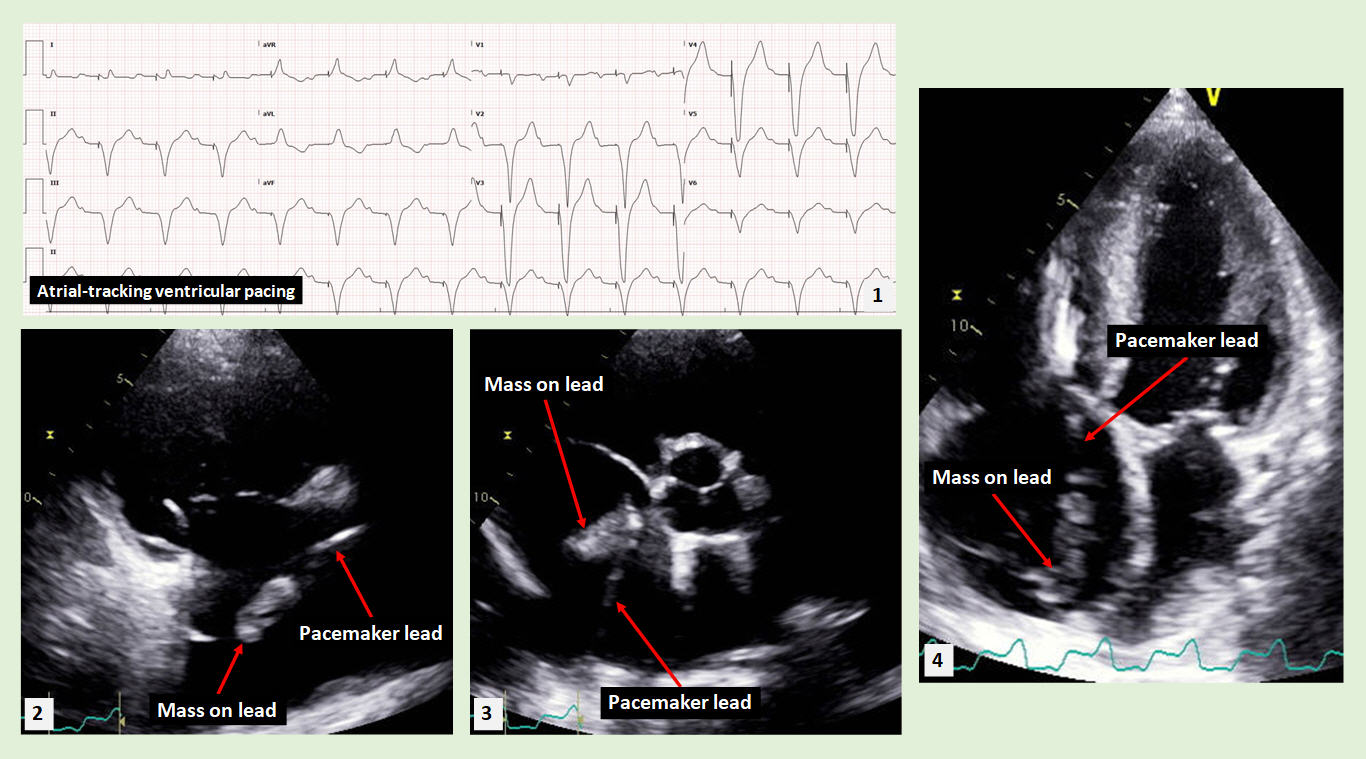
Figure 1 shows an electrocardiogram (EKG) revealing sinus rhythm with atrial tracking ventricular pacing. Figure 2 is a 2-dimensional transthoracic echocardiogram (2-D TTE) view in the modified parasternal long axis view across the right atrium and right ventricular inflow. It shows an atrial pacemaker lead with a mobile mass attached to the lead (see accompanying video). Figure 3 demonstrates the mass on the pacemaker lead within the right atrium in a 2-D parasternal short axis view at the level of the aortic valve. Figure 4 is an apical 4-chamber view demonstrating the left atrial and left ventricular pacemaker leads with a mass adherent to the atrial lead. The mass adherent to the pacemaker lead has the consistency of thrombus, and in the absence of signs and symptoms of infection, it was treated with anticoagulation.
Discussion
Pacemaker leads are prone to developing thrombi which can appear as an oscillating mass adherent to the lead mimicking an infection on echocardiography [1]. Differentiation between a thrombus and vegetation may be difficult and can be helped by the use of 18F-fluorodeoxyglucose positron emission tomography/computed tomography [2].
Echocardiography remains the gold standard for diagnosing pacemaker lead thrombi. Using echocardiography, the size, motion, potential complications such as embolization or obstruction of cardiac valves can be characterized, and may help guide management [3]. Pacemaker lead thrombi can sometimes also be visualized and diagnosed by cardiac computed tomography [4].
Large thrombi attached to a pacemaker lead have been reported to result in pulmonary embolism [5]. However, the risk of embolization due to pacemaker lead thrombi appears to be small compared to the overall prevalence of these thrombi [6].
The overall incidence of pacemaker lead thrombosis remains low; treatment with anticoagulation is recommended especially prior to ablation procedures [7]. One important risk factor for developing such thrombi seems to be the presence of atrial fibrillation [8].
When an adherent thrombus is large and causing significant embolization or obstruction of the tricuspid valve inflow [9] percutaneous removal of the right-sided leads is often needed [10]. Potential complications with percutaneous approach of lead removal have been reported, including bleeding, tamponade and infection, which may necessitate surgical intervention [11].
References:
Authors:
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulik Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Figure 1 shows an electrocardiogram (EKG) revealing sinus rhythm with atrial tracking ventricular pacing. Figure 2 is a 2-dimensional transthoracic echocardiogram (2-D TTE) view in the modified parasternal long axis view across the right atrium and right ventricular inflow. It shows an atrial pacemaker lead with a mobile mass attached to the lead (see accompanying video). Figure 3 demonstrates the mass on the pacemaker lead within the right atrium in a 2-D parasternal short axis view at the level of the aortic valve. Figure 4 is an apical 4-chamber view demonstrating the left atrial and left ventricular pacemaker leads with a mass adherent to the atrial lead. The mass adherent to the pacemaker lead has the consistency of thrombus, and in the absence of signs and symptoms of infection, it was treated with anticoagulation.
Discussion
Pacemaker leads are prone to developing thrombi which can appear as an oscillating mass adherent to the lead mimicking an infection on echocardiography [1]. Differentiation between a thrombus and vegetation may be difficult and can be helped by the use of 18F-fluorodeoxyglucose positron emission tomography/computed tomography [2].
Echocardiography remains the gold standard for diagnosing pacemaker lead thrombi. Using echocardiography, the size, motion, potential complications such as embolization or obstruction of cardiac valves can be characterized, and may help guide management [3]. Pacemaker lead thrombi can sometimes also be visualized and diagnosed by cardiac computed tomography [4].
Large thrombi attached to a pacemaker lead have been reported to result in pulmonary embolism [5]. However, the risk of embolization due to pacemaker lead thrombi appears to be small compared to the overall prevalence of these thrombi [6].
The overall incidence of pacemaker lead thrombosis remains low; treatment with anticoagulation is recommended especially prior to ablation procedures [7]. One important risk factor for developing such thrombi seems to be the presence of atrial fibrillation [8].
When an adherent thrombus is large and causing significant embolization or obstruction of the tricuspid valve inflow [9] percutaneous removal of the right-sided leads is often needed [10]. Potential complications with percutaneous approach of lead removal have been reported, including bleeding, tamponade and infection, which may necessitate surgical intervention [11].
References:
- Panagiotis MN, Nikolaos MP, St Georgia G, Athanasios KI. Case report: recurrent thrombosis of an old lead of a DDDR pacemaker mimicking lead infection. Eur Heart J Case Rep. 2018 May 26;2(2):yty063.
- Salaun E, Deharo JC, Casalta JP, Franceschi F, Hubert S, Renard S, Riberi A, Avierinos JF, Habib G. An Oscillating Mass Attached to a Pacemaker Lead: Thrombus or Vegetation? A Fishing Story. JACC Clin Electrophysiol. 2017 Aug;3(8):915-916.
- Raut MS, Maheshwari A, Dubey S. Thrombus on pacemaker lead. Indian Heart J. 2015 Dec;67 Suppl 3(Suppl 3):S120-1.
- Lin KF, Wu FZ. Large right atrial pacemaker lead thrombus diagnosed by chest CT angiography. Postgrad Med J. 2017 Feb;93(1096):109-110.
- D'Aloia A, Bonadei I, Vizzardi E, Curnis A. Right giant atrial thrombosis and pulmonary embolism complicating pacemaker leads. BMJ Case Rep. 2013 Aug 30;2013:bcr2012008017.
- Noheria A, Ponamgi SP, Desimone CV, Vaidya VR, Aakre CA, Ebrille E, Hu T, Hodge DO, Slusser JP, Ammash NM, Bruce CJ, Rabinstein AA, Friedman PA, Asirvatham SJ. Pulmonary embolism in patients with transvenous cardiac implantable electronic device leads. Europace. 2016 Feb;18(2):246-52.
- Sugrue A, DeSimone CV, Lenz CJ, Packer DL, Asirvatham SJ. Mobile thrombus on cardiac implantable electronic device leads of patients undergoing cardiac ablation: incidence, management, and outcomes. J Interv Card Electrophysiol. 2016 Aug;46(2):115-20.
- Rahbar AS, Azadani PN, Thatipelli S, Fleischmann KE, Nguyen N, Lee BK. Risk factors and prognosis for clot formation on cardiac device leads. Pacing Clin Electrophysiol. 2013 Oct;36(10):1294-300.
- Tugcu A, Yildirimturk O, Tayyareci Y, Sagbas E, Yazicioglu N, Aytekin S. Right atrial pacemaker lead thrombosis causing tricuspid inflow obstruction. Pacing Clin Electrophysiol. 2009 Feb;32(2):262-4.
- Okamura H, Van Arnam JS, Aubry MC, Friedman PA, Cha YM. Successful pacemaker lead extraction involving an ossified thrombus: A case report. J Arrhythm. 2017 Apr;33(2):150-151.
- Hamid S, Arujuna A, Ginks M, McPhail M, Patel N, Bucknall C, Rinaldi C. Pacemaker and defibrillator lead extraction: predictors of mortality during follow-up. Pacing Clin Electrophysiol. 2010 Feb;33(2):209-16.
Authors:
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulik Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL