December 2019 Issue
ISSN 2689-291X
ISSN 2689-291X
Trial Review
The ISCHEMIA Trial: Is Routine Revascularization Warranted?
Abstract
Results of the ISCHEMIA study (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) were presented at the American Heart Association (AHA) Annual Scientific Sessions in November 2019 in Philadelphia [1, 2]. This National Heart/Lung/Blood Institute – funded study compared routine invasive therapy versus optimal medical therapy amongst patients with stable ischemic heart disease and moderate to severe ischemia on stress testing.
Study Design:
Results of the ISCHEMIA study (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) were presented at the American Heart Association (AHA) Annual Scientific Sessions in November 2019 in Philadelphia [1, 2]. This National Heart/Lung/Blood Institute – funded study compared routine invasive therapy versus optimal medical therapy amongst patients with stable ischemic heart disease and moderate to severe ischemia on stress testing.
Study Design:
- Randomized, parallel, international multi-center trial
- Enrolled 5179 participants; lasted for 7 years
- Routine invasive arm (PCI & CABG): 2588 subjects
- 96% catheterization; 80% revascularization
- Medical therapy: 2591 subjects
- 28% catheterization; 23% revascularization
- Age > 20 years
- Moderate to severe ischemia on noninvasive stress testing:
- Nuclear ≥ 10% ischemia
- echo ≥ 3 segments of ischemia
- CMR ≥ 12% ischemia and/or ≥ 3 segments with ischemia
- GXT ≥ 1.5 mm ST depression in ≥ 2 leads or ≥ 2 mm ST depression in single lead at < 7 METs with angina
- Left main ≥ 50% stenosis
- GFR < 30 ml/min
- Recent MI
- EF < 35%
- Left main stenosis >50%
- Advanced angina at baseline
- NYHA III-IV heart failure
- PCI or CABG within last year
|
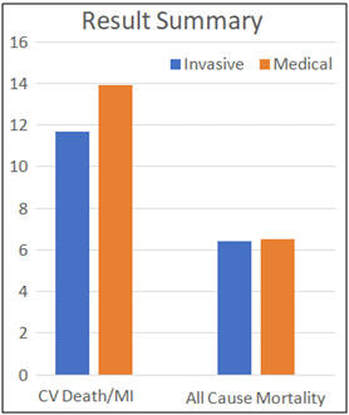
Results
Primary outcome: Cardiovascular (CV) death, myocardial infarction (MI), resuscitated cardiac arrest, hospitalization for unstable angina or heart failure at 3.3 years:
|
Discussion
The data from ISCHEMIA trial demonstrates that in stable ischemic heart disease and moderate to severe ischemia on noninvasive testing, routine catheterization and revascularization do not reduce major adverse cardiovascular events when compared to optimal medical therapy alone. However, these results cannot be applied to patients who met exclusion criteria of the study, such as more than 50% left main disease, GFR < 30 ml/min, recent ACS, EF < 35%, unacceptable angina at baseline, NYHA Class III – IV heart failure, or revascularization within the preceding year.
The results of the ISCHEMIA trial may not be surprising in light of similar findings from other clinical trials such as the COURAGE trial [3], with its sustained findings up to 15 years [4]. It does, however, present incremental evidence in a larger number of patients that optimal medical therapy remains the cornerstone of treating stable ischemic heart disease, even in the presence of moderate to severe ischemia demonstrated on noninvasive testing (excluding ACS situations).
Clinical Implications
The field of interventional cardiology has evolved exponentially ever since its inception greater than 40 years ago [5]. This was paralleled by concomitant rapid development of medical therapy which repeatedly proved to be equally protective to PCI or even CABG, especially in patients with stable ischemic heart disease [6, 7, 8]. With these results, cardiologists should focus on aggressive risk factors modification and optimization of medical therapy prior to sending their patients to the catheterization lab, where the main utility is for symptom relief (i.e. those who have failed medical therapy) rather than survival benefit in this population [9].
References
Authors:
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The data from ISCHEMIA trial demonstrates that in stable ischemic heart disease and moderate to severe ischemia on noninvasive testing, routine catheterization and revascularization do not reduce major adverse cardiovascular events when compared to optimal medical therapy alone. However, these results cannot be applied to patients who met exclusion criteria of the study, such as more than 50% left main disease, GFR < 30 ml/min, recent ACS, EF < 35%, unacceptable angina at baseline, NYHA Class III – IV heart failure, or revascularization within the preceding year.
The results of the ISCHEMIA trial may not be surprising in light of similar findings from other clinical trials such as the COURAGE trial [3], with its sustained findings up to 15 years [4]. It does, however, present incremental evidence in a larger number of patients that optimal medical therapy remains the cornerstone of treating stable ischemic heart disease, even in the presence of moderate to severe ischemia demonstrated on noninvasive testing (excluding ACS situations).
Clinical Implications
The field of interventional cardiology has evolved exponentially ever since its inception greater than 40 years ago [5]. This was paralleled by concomitant rapid development of medical therapy which repeatedly proved to be equally protective to PCI or even CABG, especially in patients with stable ischemic heart disease [6, 7, 8]. With these results, cardiologists should focus on aggressive risk factors modification and optimization of medical therapy prior to sending their patients to the catheterization lab, where the main utility is for symptom relief (i.e. those who have failed medical therapy) rather than survival benefit in this population [9].
References
- www.ischemiatrial.org
- ISCHEMIA – International Study of Comparative Health Effectiveness with Medical and Invasive Approaches: Primary Report of Clinical Outcomes. Presented by Judith S. Hochman, NYU School of Medicine, NY at the American Heart Association Annual Scientific Sessions (AHA 2019) in Philadelphia, PA on November 16, 2019.
- Boden W, O'Rourke R, Teo K, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007 Apr 12;356(15):1503-16.
- Sedlis S, Hartigan P, Teo K, et al. Effect of PCI on Long-Term Survival in Patients with Stable Ischemic Heart Disease. N Engl J Med. 2015 Nov 12;373(20):1937- 46.
- Sachdev S, Tahir H, Awan GM, Omar B. Angioplasty Beginnings..40 Years Later. Cardiofel Newslet 2018 September;1(3):17-18.
- Hueb W, Lopes N, Gersh B, et al. Ten-year follow-up survival of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation. 2010 Sep 7;122(10):949-57.
- Velazquez EJ, Lee KL, Deja MA, et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011 Apr 28;364(17):1607-16.
- Al-Lamee R, Thompson D, Dehbi HM, et al. Percutaneous coronary intervention in stable angina (ORBITA): a double-blind, randomised controlled trial. Lancet. 2018 Jan 6;391(10115):31-40.
- Torosoff M, Sidhu M, Desai K, et al. Revascularization options in stable coronary artery disease: it is not how to revascularize, it is whether and when to revascularize. J Comp Eff Res. 2015 Sep;4(5):505-14.
Authors:
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL