December 2022 Issue
ISSN 2689-291X
ISSN 2689-291X
Right-Sided Defibrillator:
Elevated Defibrillation Threshold!
Description
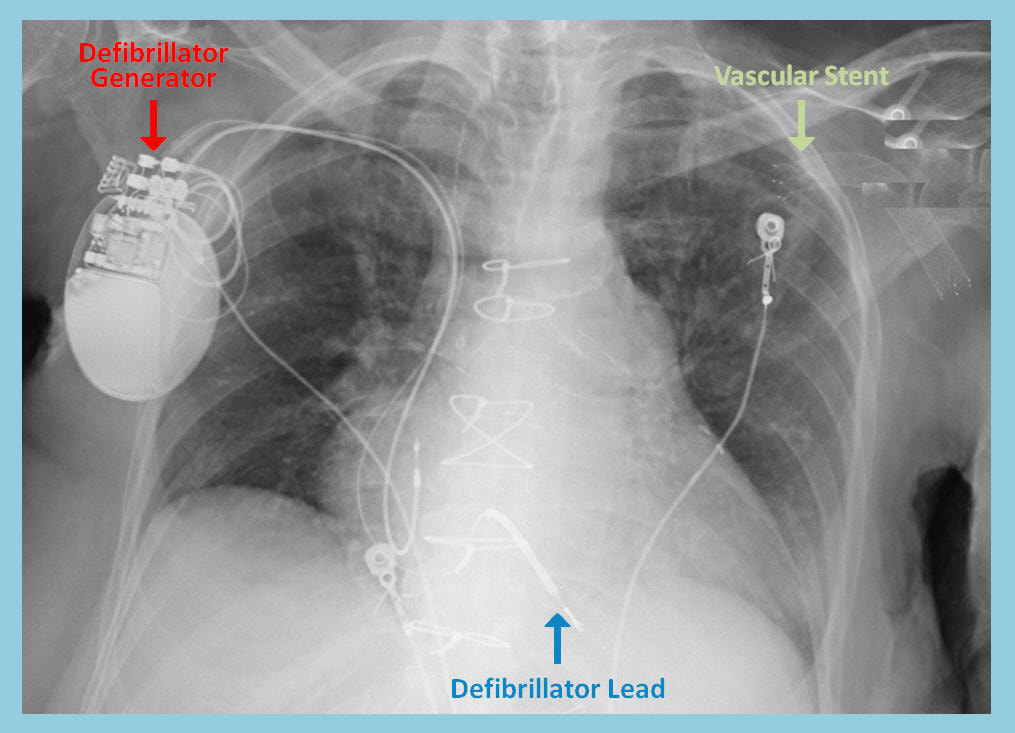
The above chest x ray reveals an implantable cardioverter defibrillator (ICD) device implanted in the setting of prior coronary artery bypass graft surgery (CABG) and ischemic cardiomyopathy in a hemodialysis patient with a left upper arm hemodialysis graft. Stent placement within the dialysis graft is noted. The ICD generator box, as shown, was thereby implanted in the right upper chest to avoid the left-sided vasculature and prevent interference with the hemodialysis access. The defibrillation axis between the defibrillator lead shown and the ICD generator is therefore rightward and opposite to the conventional left-sided implanted ICD generators. This configuration can potentially lead to unsuccessful defibrillation due to inadequate capture of the ventricles by the defibrillation current. Thus, such unconventional ICD implantation requires meticulous testing of the defibrillation thresholds intraoperatively.
Discussion
The prevalence of coronary artery disease and cardiomyopathy, with their inherent risk of causing fatal ventricular arrhythmia, has resulted in broad indications and increased use of ICD therapy for the prevention of sudden cardiac death [1, 2]. Vascular anomalies, whether congenital [3] or acquired [4], present challenges to traditional device insertion, with potential complications involving the subclavian veins [5]. Newer technologies such as leadless pacemakers [6] and subcutaneous ICDs [7] offer promise for hemodialysis patients requiring implantable pacemakers or defibrillators.
ICD placement, however, can be more challenging as the direction of the defibrillation current between the right ventricular lead and the generator box is an important factor in determining successful capture of the ventricles and termination of an arrhythmia. This mandates thorough testing of defibrillation thresholds in patients undergoing subcutaneous ICD implantation [8].
The right-sided implantation of the defibrillator generator, as demonstrated in the image above, causes disturbance of the current waveform [9], which result in increased defibrillation threshold [10]. Optimization of the defibrillation vector [11] and intraoperative testing of the defibrillation thresholds are recommended to assure successful current delivery [12].
References
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Alexis Parks, D.O.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The above chest x ray reveals an implantable cardioverter defibrillator (ICD) device implanted in the setting of prior coronary artery bypass graft surgery (CABG) and ischemic cardiomyopathy in a hemodialysis patient with a left upper arm hemodialysis graft. Stent placement within the dialysis graft is noted. The ICD generator box, as shown, was thereby implanted in the right upper chest to avoid the left-sided vasculature and prevent interference with the hemodialysis access. The defibrillation axis between the defibrillator lead shown and the ICD generator is therefore rightward and opposite to the conventional left-sided implanted ICD generators. This configuration can potentially lead to unsuccessful defibrillation due to inadequate capture of the ventricles by the defibrillation current. Thus, such unconventional ICD implantation requires meticulous testing of the defibrillation thresholds intraoperatively.
Discussion
The prevalence of coronary artery disease and cardiomyopathy, with their inherent risk of causing fatal ventricular arrhythmia, has resulted in broad indications and increased use of ICD therapy for the prevention of sudden cardiac death [1, 2]. Vascular anomalies, whether congenital [3] or acquired [4], present challenges to traditional device insertion, with potential complications involving the subclavian veins [5]. Newer technologies such as leadless pacemakers [6] and subcutaneous ICDs [7] offer promise for hemodialysis patients requiring implantable pacemakers or defibrillators.
ICD placement, however, can be more challenging as the direction of the defibrillation current between the right ventricular lead and the generator box is an important factor in determining successful capture of the ventricles and termination of an arrhythmia. This mandates thorough testing of defibrillation thresholds in patients undergoing subcutaneous ICD implantation [8].
The right-sided implantation of the defibrillator generator, as demonstrated in the image above, causes disturbance of the current waveform [9], which result in increased defibrillation threshold [10]. Optimization of the defibrillation vector [11] and intraoperative testing of the defibrillation thresholds are recommended to assure successful current delivery [12].
References
- Meyer C, Schueller P, Rodenbeck A, et al. Primary and secondary prevention of ventricular arrhythmias in dilated cardiomyopathy: nonsustained, sustained, and incessant. Int Heart J. 2009 Nov;50(6):741-51.
- Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2018 Oct 2;72(14):e91-e220.
- Riad M, Rahman M, Bardia N, et al. Implantable Cardiac Defibrillator Insertion Challenges In Vascular Anomalies. J Am Coll Cardiol. 2023 Mar, 81 (8_Supplement) 3241.
- Duckett SG, Kalra P, Farrell TG. Limited venous access and pacemaker insertion in a haemodialysis patient: case report. Int J Cardiol. 2010 Jan 7;138(1):e4-5.
- Teruya TH, Abou-Zamzam AM Jr, Limm W, et al. Symptomatic subclavian vein stenosis and occlusion in hemodialysis patients with transvenous pacemakers. Ann Vasc Surg. 2003 Sep;17(5):526-9.
- Bednarczyk D, Kuliczkowski W, Letachowicz K, et al. Simultaneous placement of leadless pacemaker and dialysis catheter in patient with exhausted vasculature. J Vasc Access. 2021 Jan;22(1):147-150.
- Pun PH, Parzynski CS, Friedman DJ, Sanders et al. Trends in Use and In-Hospital Outcomes of Subcutaneous Implantable Cardioverter Defibrillators in Patients Undergoing Long-Term Dialysis. Clin J Am Soc Nephrol. 2020 Nov 6;15(11):1622-1630.
- le Polain de Waroux JB, Ploux S, Mondoly P, et al. Defibrillation testing is mandatory in patients with subcutaneous implantable cardioverter-defibrillator to confirm appropriate ventricular fibrillation detection. Heart Rhythm. 2018 May;15(5):642-650.
- Varma N, Schaerf R, Kalbfleisch S, et al. Defibrillation thresholds with right pectoral implantable cardioverter defibrillators and impact of waveform tuning (the Tilt and Tune trial). Europace. 2017 Nov 1;19(11):1810-1817.
- Friedman PA, Rasmussen MJ, Grice S, et al. Defibrillation thresholds are increased by right-sided implantation of totally transvenous implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 1999 Aug;22(8):1186-92.
- Patton K, Reddy VY. Optimizing the defibrillation vector with a right-sided implantable cardioverter-defibrillator. Heart Rhythm. 2004 Dec;1(6):756.
- Keyser A, Hilker MK, Ucer E, et al. Significance of intraoperative testing in right-sided implantable cardioverter-defibrillators. J Cardiothorac Surg. 2013 Apr 11;8:77.
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Alexis Parks, D.O.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL