December 2023 Issue
ISSN 2689-291X
ISSN 2689-291X
STEMI or NSTEMI? –
Sequential Limb Lead Misplacement!
Description
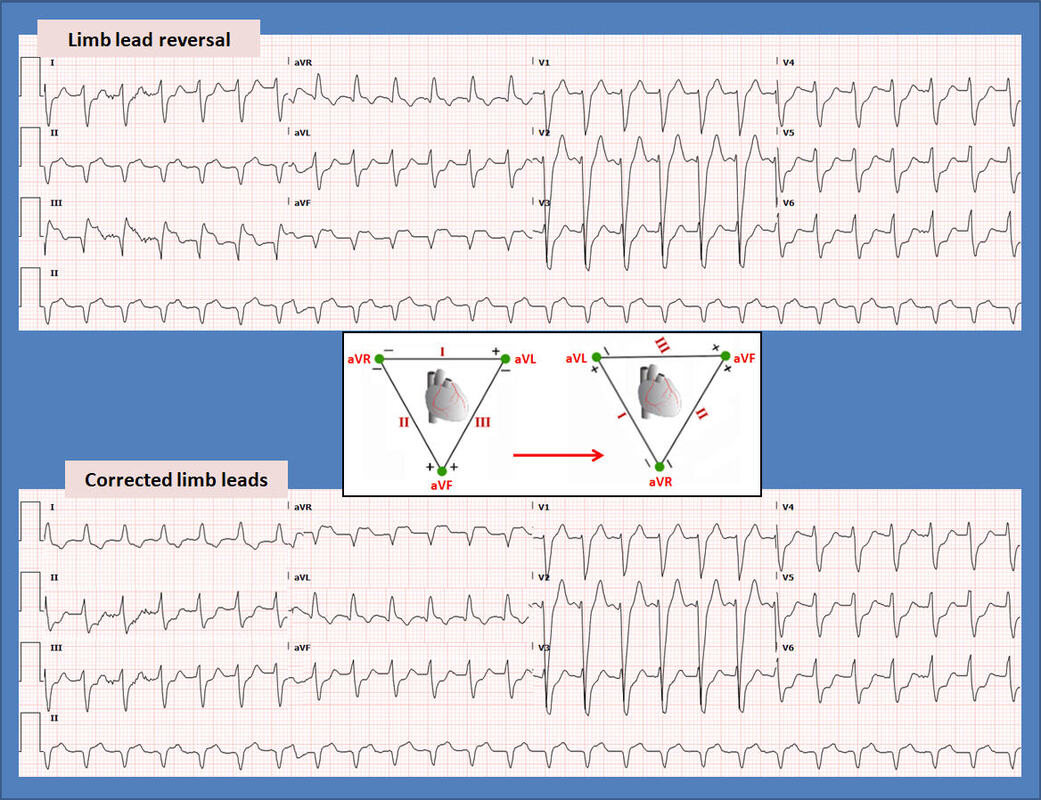
The top panel electrocardiogram (ECG) above reveals sinus tachycardia, intraventricular conduction delay (atypical left bundle branch block), lateral ST-segment depressions and inferior ST-segment elevations suggestive of an acute inferior myocardial infarction, prompting a STEMI code. When compared to a prior ECG, lead misplacement was suspected which prompted an immediate repeat of the ECG shown in the lower panel, with correct leads.
In examining both EKGs, a simple lead reversal could not explain the difference. However, utilizing an Einthoven’s triangle drawing, it became apparent that there was a sequential limb lead misplacement (see insert). As can be seen, Lead III on the corrected ECG corresponds to lead I on the reversed ECG (with similar polarity). Lead II on the corrected ECG reflect Lead III on the reversed ECG with inverse polarity (upside down). Lead I on the corrected ECG reflects lead II on the reversed ECG with inverse polarity (upside down). The multiple lead reversals resulted in a sequential limb lead misplacement artifact causing the erroneous appearance of inferior STEMI.
Discussion
ECG recoding artifacts are reported in 5.9% to 6.5% of ECGs performed in a hospital setting [1, 2]. Out of these 20% – 30% represent either lead misplacement or lead reversal which can lead to misinterpretation of the ECG.
ECG lead reversal can be caused by and isolated improper lead placement at the chest level due to operator error. Less often lead reversals can be caused by a faulty connection of the cable junction which can propagate the error in many ECGs until the connection is fixed [3, 4].
Current ECG machine software has a limited ability to detect more than basic lead reversals, such as arm lead reversal. Solving the puzzle of which leads were reversed is an important intriguing exercise [5] which can help reconstruct the true findings in case a repeat ECG can be timely performed. Using Einthoven’s transparency [6] as demonstrated in the above image can often help decipher the puzzle. Hopefully artificial intelligence can be employed in the future to help better identify ECG recording errors in a timely manner [7].
References
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Brent Ruiz, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hajira Malik, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Celestine Odigwe, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
The top panel electrocardiogram (ECG) above reveals sinus tachycardia, intraventricular conduction delay (atypical left bundle branch block), lateral ST-segment depressions and inferior ST-segment elevations suggestive of an acute inferior myocardial infarction, prompting a STEMI code. When compared to a prior ECG, lead misplacement was suspected which prompted an immediate repeat of the ECG shown in the lower panel, with correct leads.
In examining both EKGs, a simple lead reversal could not explain the difference. However, utilizing an Einthoven’s triangle drawing, it became apparent that there was a sequential limb lead misplacement (see insert). As can be seen, Lead III on the corrected ECG corresponds to lead I on the reversed ECG (with similar polarity). Lead II on the corrected ECG reflect Lead III on the reversed ECG with inverse polarity (upside down). Lead I on the corrected ECG reflects lead II on the reversed ECG with inverse polarity (upside down). The multiple lead reversals resulted in a sequential limb lead misplacement artifact causing the erroneous appearance of inferior STEMI.
Discussion
ECG recoding artifacts are reported in 5.9% to 6.5% of ECGs performed in a hospital setting [1, 2]. Out of these 20% – 30% represent either lead misplacement or lead reversal which can lead to misinterpretation of the ECG.
ECG lead reversal can be caused by and isolated improper lead placement at the chest level due to operator error. Less often lead reversals can be caused by a faulty connection of the cable junction which can propagate the error in many ECGs until the connection is fixed [3, 4].
Current ECG machine software has a limited ability to detect more than basic lead reversals, such as arm lead reversal. Solving the puzzle of which leads were reversed is an important intriguing exercise [5] which can help reconstruct the true findings in case a repeat ECG can be timely performed. Using Einthoven’s transparency [6] as demonstrated in the above image can often help decipher the puzzle. Hopefully artificial intelligence can be employed in the future to help better identify ECG recording errors in a timely manner [7].
References
- Moses A, Malozzi C, Omar B. Prevalence of ECG Recording Errors in a University Hospital ECG Database. Circulation: Cardiovascular Quality and Outcomes. 2016;9:A236.
- Awan M, Omar M, Omar B, Malozzi C, Awan GM ECG Recording Errors Prevalence in a Hospital Setting. Circulation: Cardiovascular Quality and Outcomes. 2018;11:A244.
- Ravi R, Aravind C, Sundararajan V, Elakkumanan LB. Diagnosis and practical implications of ECG lead reversal: Anesthesiologist perspective. J Anaesthesiol Clin Pharmacol. 2021 Apr-Jun;37(2):311-312.
- Velagapudi P, Turagam MK, Ritter S, Dohrmann ML. Left arm/left leg lead reversals at the cable junction box: A cause for an epidemic of errors. J Electrocardiol. 2017 Jan-Feb;50(1):111-114.
- Sakaguchi S, Sandberg J, Benditt DG. ECG electrode reversals: An opportunity to learn from mistakes. J Cardiovasc Electrophysiol. 2018 May;29(5):806-815.
- Abi-Saleh B, Omar B. Einthoven's triangle transparency: a practical method to explain limb lead configuration following single lead misplacements. Rev Cardiovasc Med. 2010 Winter;11(1):33-8.
- Martínez-Sellés M, Marina-Breysse M. Current and Future Use of Artificial Intelligence in Electrocardiography. J Cardiovasc Dev Dis. 2023 Apr 17;10(4):175.
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Brent Ruiz, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hajira Malik, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Celestine Odigwe, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL