December 2024 Issue
ISSN 2689-291X
ISSN 2689-291X
Electrocardiographic Tremor Artifact:
Pseudo Atrial Fibrillation/Flutter!
Description
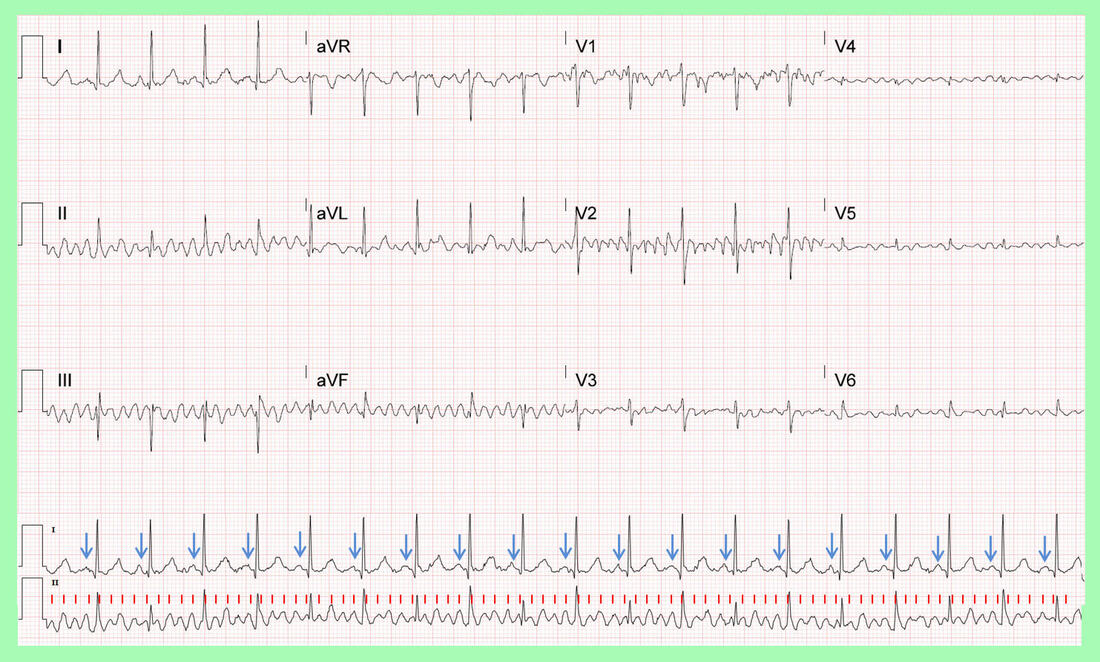
The above electrocardiogram (ECG) was performed in the setting of shivering and upper respiratory tract infection (URI). It reveals fibrillatory waves (red lines) at an atrial rate of approximately 550 beats per minute (BPM). This was concerning for atrial fibrillation or fast atrial flutter (which was the automated reading by the ECG machine), with a regular ventricular response at 116 BPM.
Closer examination of the ECG tracing, however, reveals discrete P waves in lead I (blue arrows) at an atrial rate of 116 BPM, matching the ventricular rate, indicative of sinus tachycardia. The fibrillatory waves were attributed to a tremor artifact due to the URI, mimicking atrial fibrillation/flutter as misinterpreted by the EKG machine.
Discussion
For over 100 years, the electrocardiogram has emerged as an invaluable and highly cost-effective tool in cardiology for diagnosis, risk stratification, prognostication and treatment or toxicity monitoring [1]. Nevertheless, the technology has been fraught with various intrinsic and extrinsic recording and interpretation errors and artifacts which may lead to inappropriate diagnosis and therapeutic decisions if not recognized and corrected.
Lead misplacement errors have been reported with a frequency of 6 – 7 % in a hospital setting [2, 3], often caused by an extrinsic error related to faulty lead placement. Intrinsic errors can be related to implanted devices causing the appearance of an arrhythmia, such are a bladder pacemaker [4], or inability to detect pacemaker spikes in certain devices [5].
While arm lead reversals are among the most common and easily recognizable lead placement errors [6], even by automated ECG machine readings, other precordial lead reversal may not be as obvious and will require closer scrutiny [7]. Baseline artifacts often triggered by tremor can mimic atrial flutter [8] in addition to atrial fibrillation and ventricular arrhythmia [9]. It is imperative to recognize such ECG artifacts to avoid an erroneous diagnosis which may lead to inappropriate treatments such as unnecessary anticoagulation.
References
The above electrocardiogram (ECG) was performed in the setting of shivering and upper respiratory tract infection (URI). It reveals fibrillatory waves (red lines) at an atrial rate of approximately 550 beats per minute (BPM). This was concerning for atrial fibrillation or fast atrial flutter (which was the automated reading by the ECG machine), with a regular ventricular response at 116 BPM.
Closer examination of the ECG tracing, however, reveals discrete P waves in lead I (blue arrows) at an atrial rate of 116 BPM, matching the ventricular rate, indicative of sinus tachycardia. The fibrillatory waves were attributed to a tremor artifact due to the URI, mimicking atrial fibrillation/flutter as misinterpreted by the EKG machine.
Discussion
For over 100 years, the electrocardiogram has emerged as an invaluable and highly cost-effective tool in cardiology for diagnosis, risk stratification, prognostication and treatment or toxicity monitoring [1]. Nevertheless, the technology has been fraught with various intrinsic and extrinsic recording and interpretation errors and artifacts which may lead to inappropriate diagnosis and therapeutic decisions if not recognized and corrected.
Lead misplacement errors have been reported with a frequency of 6 – 7 % in a hospital setting [2, 3], often caused by an extrinsic error related to faulty lead placement. Intrinsic errors can be related to implanted devices causing the appearance of an arrhythmia, such are a bladder pacemaker [4], or inability to detect pacemaker spikes in certain devices [5].
While arm lead reversals are among the most common and easily recognizable lead placement errors [6], even by automated ECG machine readings, other precordial lead reversal may not be as obvious and will require closer scrutiny [7]. Baseline artifacts often triggered by tremor can mimic atrial flutter [8] in addition to atrial fibrillation and ventricular arrhythmia [9]. It is imperative to recognize such ECG artifacts to avoid an erroneous diagnosis which may lead to inappropriate treatments such as unnecessary anticoagulation.
References
- Friedman PA. The Electrocardiogram at 100 Years: History and Future. Circulation. 2024 Feb 6;149(6):411-413.
- Awan M, Omar M, Omar B, Malozzi M, Awan A. ECG Recording Errors Prevalence in a Hospital Setting. Circulation: Cardiovascular Quality and Outcomes. Volume 11, Number suppl_1. 244.
- Moses A, Malozzi m, Omar B. Prevalence of ECG Recording Errors in a University Hospital ECG Database. Circulation: Cardiovascular Quality and Outcomes. Volume 9, Number suppl_2. 236.
- Mulyala A, Shah N, Riad M, Bardia N, Sarwar U, Patel M, Rahman MU, Malozzi C, Omar B. Bladder Pacemaker: Electrocardiographic Interference! Cardiofel Newslet 2022. Nov; 5(11):34 – 35.
- Ruiz B, Odigwe C, Malik H, Rahman M, Riad M, Manoharan S, Malozzi C, Omar B. Invisible Pacing Spikes: Pseudo LBBB! Cardiofel Newslet 2024. Oct; 7(10):24– 25.
- Rahman M, Riad M, Shah N, Odigwe C, Ruiz B, Malik H, Omar B, Malozzi C. Arm Lead Reversal Look-Alike: Grounding Artifact! Cardiofel Newslet 2024. June; 7(6):15 – 16.
- Abi-Saleh B, Omar B. Einthoven's triangle transparency: a practical method to explain limb lead configuration following single lead misplacements. Rev Cardiovasc Med. 2010 Winter;11(1):33-8.
- Papanastasiou CA, Petroglou D, Palaiodimos L, Economou F. A Rare Case of Pseudo-atrial Flutter Waves in a Patient with Essential Tremor. Cureus. 2019 Jan 21;11(1):e3934.
- Hwang WJ, Chen JY, Sung PS, Lee JC. Parkinsonian tremor-induced electrocardiographic artifacts mimicking atrial flutter/fibrillation or ventricular tachycardia. Int J Cardiol. 2014 May 15;173(3):597-600.
Authors:
Mohammad As Sayaideh, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Brent Ruiz, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Celestine Odigwe, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sanchitha Nagaraj, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Alexis Parks, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hajira Malik, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Suganya Manoharan, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Mohammad As Sayaideh, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Brent Ruiz, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Celestine Odigwe, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sanchitha Nagaraj, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Alexis Parks, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hajira Malik, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Suganya Manoharan, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL