February 2020 Issue
ISSN 2689-291X
ISSN 2689-291X
Challenging Images
Thoracic Aortic Repair..TEVAR or TOVAR, That Is The Question!
Description
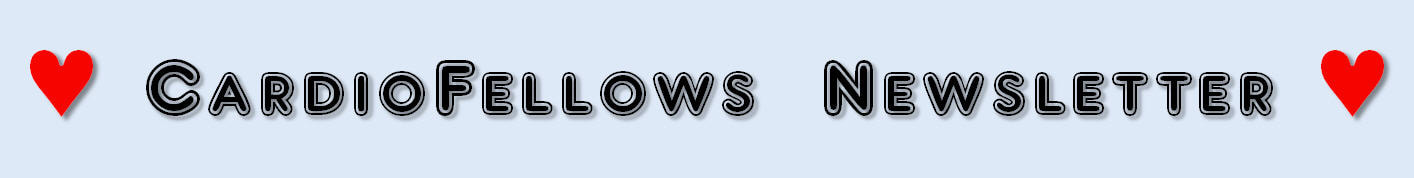
The figure above shows chest X ray (A & B) and computed tomography (CT) images (C & D) of the chest before (A & C) and after (B & D) thoracic endovascular aortic repair (TEVAR) with a stent graft for aortic arch aneurysm and penetrating ulcer of the descending thoracic aorta.
Discussion
Thoracic aortic aneurysm (TAA) is an abnormal dilatation of any of the three segments of the thoracic aorta; ascending, arch or descending thoracic aorta. When the aorta is abnormally enlarged, it can lead to fatal rupture if not immediately diagnosed and treated. With an incidence of roughly 10 cases per 100,000, TAAs are more prevalent in men, but have worse prognosis in women [1].
There are many risk factors for TAA, including poorly controlled hypertension, stimulant use (e.g. cocaine), genetic syndromes (Marfan syndrome, Turner syndrome, Loeys-Dietz syndrome), inflammatory vasculitides (Behcet syndrome, Takayasu arteritis) and chronic corticosteroid use [1].
Aneurysm size predicts growth rate and the risk of rupture. Overall, the survival of patients with an aneurysm > 5 cm in diameter is poorer than in patients with aneurysms of smaller diameter. The cut point for intervention on TAAs is a diameter of 5.5 cm, due to the significant risk of rupture when the diameter is larger, or when the rate of growth of the aneurysm equals to or exceeds 0.5 cm per year. Intervention can be accomplished by Thoracic Open Vascular Aortic Repair (TOVAR) versus Thoracic EndoVascular Aortic Repair (TEVAR); either of which is often decided based on the patient’s overall surgical risk [2].
Historically, repair of TAA syndromes involved the use of open surgery (TOVAR). However, long term outcomes such as increased risk of peri-operative mortality, expense and prolonged hospital course ushered the need for more conservative approaches. Parodi et al. in 1991 pioneered the concept of TEVAR testing on animals, and with improved outcomes, they were able to acquire FDA approval for TEVAR as the standard of care for many thoracic aortic syndromes traditionally treated by open surgical repair [3, 4].
Recent studies challenged the superiority of outcomes using TEVAR. Although TEVAR resulted in less peri-operative mortality, one study reported that Medicare patients who underwent TEVAR had lower survival long-term (likely a reflection of their higher risk) compared with patients who were selected for open surgical repair [5]. Nevertheless, TEVAR remains an attractive less invasive option for many aortic syndromes. Although it was initially used to treat aortic aneurysms, TEVAR indications currently include treating type B aortic dissections (with malperfusion or rupture), acute aortic transections due to trauma, and penetrating aortic ulcers, as demonstrated in the figure above [6].
References:
Authors:
Nneka Nwokeocha, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The figure above shows chest X ray (A & B) and computed tomography (CT) images (C & D) of the chest before (A & C) and after (B & D) thoracic endovascular aortic repair (TEVAR) with a stent graft for aortic arch aneurysm and penetrating ulcer of the descending thoracic aorta.
Discussion
Thoracic aortic aneurysm (TAA) is an abnormal dilatation of any of the three segments of the thoracic aorta; ascending, arch or descending thoracic aorta. When the aorta is abnormally enlarged, it can lead to fatal rupture if not immediately diagnosed and treated. With an incidence of roughly 10 cases per 100,000, TAAs are more prevalent in men, but have worse prognosis in women [1].
There are many risk factors for TAA, including poorly controlled hypertension, stimulant use (e.g. cocaine), genetic syndromes (Marfan syndrome, Turner syndrome, Loeys-Dietz syndrome), inflammatory vasculitides (Behcet syndrome, Takayasu arteritis) and chronic corticosteroid use [1].
Aneurysm size predicts growth rate and the risk of rupture. Overall, the survival of patients with an aneurysm > 5 cm in diameter is poorer than in patients with aneurysms of smaller diameter. The cut point for intervention on TAAs is a diameter of 5.5 cm, due to the significant risk of rupture when the diameter is larger, or when the rate of growth of the aneurysm equals to or exceeds 0.5 cm per year. Intervention can be accomplished by Thoracic Open Vascular Aortic Repair (TOVAR) versus Thoracic EndoVascular Aortic Repair (TEVAR); either of which is often decided based on the patient’s overall surgical risk [2].
Historically, repair of TAA syndromes involved the use of open surgery (TOVAR). However, long term outcomes such as increased risk of peri-operative mortality, expense and prolonged hospital course ushered the need for more conservative approaches. Parodi et al. in 1991 pioneered the concept of TEVAR testing on animals, and with improved outcomes, they were able to acquire FDA approval for TEVAR as the standard of care for many thoracic aortic syndromes traditionally treated by open surgical repair [3, 4].
Recent studies challenged the superiority of outcomes using TEVAR. Although TEVAR resulted in less peri-operative mortality, one study reported that Medicare patients who underwent TEVAR had lower survival long-term (likely a reflection of their higher risk) compared with patients who were selected for open surgical repair [5]. Nevertheless, TEVAR remains an attractive less invasive option for many aortic syndromes. Although it was initially used to treat aortic aneurysms, TEVAR indications currently include treating type B aortic dissections (with malperfusion or rupture), acute aortic transections due to trauma, and penetrating aortic ulcers, as demonstrated in the figure above [6].
References:
- Hiratzka LF, Bakris GL, Beckman JA, et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM Guidelines for the diagnosis and management of patients with thoracic aortic disease. A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, American Association for Thoracic Surgery, American College of Radiology, American Stroke Association, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of Thoracic Surgeons,and Society for Vascular Medicine. J Am Coll Cardiol. 2010 Apr 6;55(14):e27-e129.
- Juvonen T, Ergin MA, Galla JD, et al. Prospective study of the natural history of thoracic aortic aneurysms. Ann Thorac Surg. 1997 Jun;63(6):1533-45.
- Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg. 1991 Nov;5(6):491-9.
- Bhamidipati CM, LaPar DJ, Mehta GS, et al. Have thoracic endografting outcomes improved since US Food and Drug Administration approval? Ann Thorac Surg. 2011 May;91(5):1314-22; discussion 1322.
- Goodney PP, Travis L, Lucas FL, Survival after open versus endovascular thoracic aortic aneurysm repair in an observational study of the Medicare population. Circulation. 2011 Dec 13;124(24):2661-9.
- Nation DA, Wang GJ. TEVAR: Endovascular Repair of the Thoracic Aorta. Semin Intervent Radiol. 2015 Sep;32(3):265-71.
Authors:
Nneka Nwokeocha, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL