January 2023 Issue
ISSN 2689-291X
ISSN 2689-291X
Brugada Phenocopy:
An Electrocardiographic Chameleon!
Description
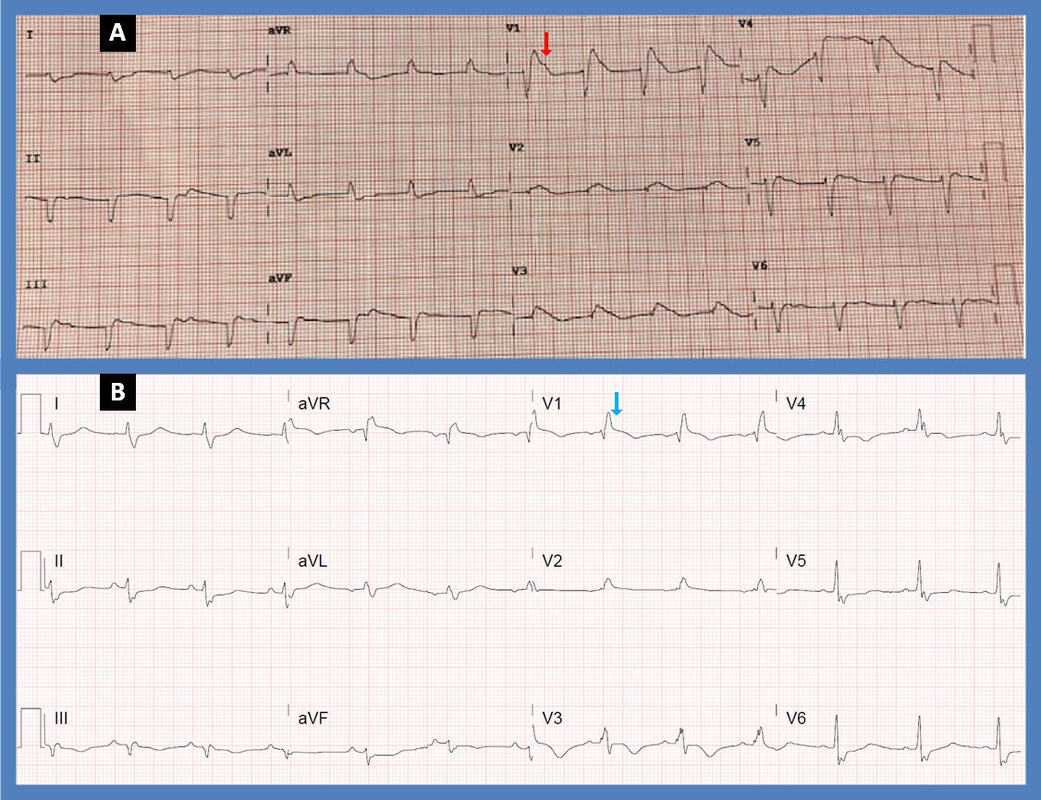
The electrocardiograms (EKG) above represent acute changes in a patient presenting with massive pulmonary embolism. There is coving of the ST segments in lead V1 followed by negative T waves (Figure A; red arrow), suggestive of Brugada pattern. Initial concern for an ST-segment elevation myocardial infarction (STEMI) necessitated a coronary angiogram which was negative for obstructive coronary disease. The EKG changes resolved following initial anticoagulant management, revealing an underlying right bundle branch block (Fig. B, blue arrow). Therefore the initial Brugada pattern was induced by the stress of the pulmonary embolus rather than heritable Brugada syndrome. This phenomenon has been described in response to variable stressors and has been termed Brugada phenocopy [1].
Discussion
There are several noncardiac conditions which can cause ST-segment elevation on EKG mimicking acute STEMI [2]. Such presentations can be challenging with need for urgent diagnostic studies to exclude obstructive coronary disease. Brugada pattern on EKG causes ST elevations in the anteroseptal leads (V1 to V2) with either coved (type I) or saddleback (type 2 and type 3) appearance of the ST segment [3].
Brugada syndrome is a highly arrhythmogenic sodium channelopathy which is autosomal dominant with incomplete penetrance. The EKG pattern, however, has also been demonstrated in patients following cocaine use, which in itself is a sodium channel blocker [4], and has been attributed to latent Brugada syndrome unmasked by sodium channel blockade. Brugada EKG pattern has also been described in the setting of flecainide use in atrial fibrillation, a class IC Vaughan-Williams classification antiarrhythmic with sodium channel blocker activity [5]. Withdrawal of flecainide normalized the EKG findings with no evidence of recurrence on ambulatory monitoring.
Beyond medications or substance use, fever of various sources has been demonstrated to induce Brugada-type EKG pattern, thought also to be secondary to unmasking of latent Brugada [6]. Although several such patients received an implantable cardioverter defibrillator, this was not associated with any significant mortality benefit.
Brugada Phenocopy is a clinical phenomenon whereby Brugada-like EKG findings appear in a patient without true congenital Brugada syndrome, and is differentiated from unmasking of true Brugada caused by sodium channel blockers [7]. In Brugada phenocopy, the distinction from true Brugada is made due to the reversibility of the EKG findings once an inciting clinical condition has resolved. For instance, recurrent hypokalemia has been demonstrated to reproduce Brugada-like EKG findings [8], in addition to other triggers such as pulmonary embolism [9] as in our case, myocardial ischemia [10], and exercise [11].
Diagnostic criteria for Brugada phenocopy to differentiate it from Brugada syndrome have been proposed [12]. First, Brugada phenocopy, in contrast to Brugada syndrome, is temporary and complete resolution of the Brugada pattern with normalization of the EKG is diagnostic. Second, Brugada phenocopy will have a low pretest probability with regards to previous cardiac arrest, family history of sudden cardiac death, or personal history of non-vagal syncope; factors which make true Brugada syndrome more likely. Finally, in Brugada phenocopy there will be a negative EKG response to sodium channel blockers, while these agents unmask Brugada EKG pattern in latent Brugada syndrome. The mechanism of Brugada phenocopy remains unclear but may involve transient phase-I ion channel imbalance of the action potential.
In conclusion, Brugada phenocopy should be an important part of the differential diagnosis in patients presenting with Brugada-type EKG abnormalities associated with several clinical conditions, as it is distinct from true heritable Brugada syndrome or unmasking of latent Brugada by sodium channel blockers [13], with a different approach to diagnosis and management. The transient EKG changes of Brugada phenocopy in response to diverse, but often intense, physiologic and pathologic stressors, mimicking the very serious and potentially fatal Brugada syndrome, are perhaps a natural environmental adaptation, an electrocardiographic chameleon, warning us that we have exhausted our natural reserves, calling for prompt action to treat such stressors and in turn reverse these EKG changes to avoid an irreversible poor outcome.
References
Authors:
Jack Galla, B.S.
Medical Student
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The electrocardiograms (EKG) above represent acute changes in a patient presenting with massive pulmonary embolism. There is coving of the ST segments in lead V1 followed by negative T waves (Figure A; red arrow), suggestive of Brugada pattern. Initial concern for an ST-segment elevation myocardial infarction (STEMI) necessitated a coronary angiogram which was negative for obstructive coronary disease. The EKG changes resolved following initial anticoagulant management, revealing an underlying right bundle branch block (Fig. B, blue arrow). Therefore the initial Brugada pattern was induced by the stress of the pulmonary embolus rather than heritable Brugada syndrome. This phenomenon has been described in response to variable stressors and has been termed Brugada phenocopy [1].
Discussion
There are several noncardiac conditions which can cause ST-segment elevation on EKG mimicking acute STEMI [2]. Such presentations can be challenging with need for urgent diagnostic studies to exclude obstructive coronary disease. Brugada pattern on EKG causes ST elevations in the anteroseptal leads (V1 to V2) with either coved (type I) or saddleback (type 2 and type 3) appearance of the ST segment [3].
Brugada syndrome is a highly arrhythmogenic sodium channelopathy which is autosomal dominant with incomplete penetrance. The EKG pattern, however, has also been demonstrated in patients following cocaine use, which in itself is a sodium channel blocker [4], and has been attributed to latent Brugada syndrome unmasked by sodium channel blockade. Brugada EKG pattern has also been described in the setting of flecainide use in atrial fibrillation, a class IC Vaughan-Williams classification antiarrhythmic with sodium channel blocker activity [5]. Withdrawal of flecainide normalized the EKG findings with no evidence of recurrence on ambulatory monitoring.
Beyond medications or substance use, fever of various sources has been demonstrated to induce Brugada-type EKG pattern, thought also to be secondary to unmasking of latent Brugada [6]. Although several such patients received an implantable cardioverter defibrillator, this was not associated with any significant mortality benefit.
Brugada Phenocopy is a clinical phenomenon whereby Brugada-like EKG findings appear in a patient without true congenital Brugada syndrome, and is differentiated from unmasking of true Brugada caused by sodium channel blockers [7]. In Brugada phenocopy, the distinction from true Brugada is made due to the reversibility of the EKG findings once an inciting clinical condition has resolved. For instance, recurrent hypokalemia has been demonstrated to reproduce Brugada-like EKG findings [8], in addition to other triggers such as pulmonary embolism [9] as in our case, myocardial ischemia [10], and exercise [11].
Diagnostic criteria for Brugada phenocopy to differentiate it from Brugada syndrome have been proposed [12]. First, Brugada phenocopy, in contrast to Brugada syndrome, is temporary and complete resolution of the Brugada pattern with normalization of the EKG is diagnostic. Second, Brugada phenocopy will have a low pretest probability with regards to previous cardiac arrest, family history of sudden cardiac death, or personal history of non-vagal syncope; factors which make true Brugada syndrome more likely. Finally, in Brugada phenocopy there will be a negative EKG response to sodium channel blockers, while these agents unmask Brugada EKG pattern in latent Brugada syndrome. The mechanism of Brugada phenocopy remains unclear but may involve transient phase-I ion channel imbalance of the action potential.
In conclusion, Brugada phenocopy should be an important part of the differential diagnosis in patients presenting with Brugada-type EKG abnormalities associated with several clinical conditions, as it is distinct from true heritable Brugada syndrome or unmasking of latent Brugada by sodium channel blockers [13], with a different approach to diagnosis and management. The transient EKG changes of Brugada phenocopy in response to diverse, but often intense, physiologic and pathologic stressors, mimicking the very serious and potentially fatal Brugada syndrome, are perhaps a natural environmental adaptation, an electrocardiographic chameleon, warning us that we have exhausted our natural reserves, calling for prompt action to treat such stressors and in turn reverse these EKG changes to avoid an irreversible poor outcome.
References
- Anselm DD, Evans JM, Baranchuk A. Brugada phenocopy: A new electrocardiogram phenomenon. World J Cardiol. 2014 Mar 26;6(3):81-6.
- Khurana KV, Ranjan A. ST-Segment Elevation in Conditions of Non-cardiovascular Origin Mimicking an Acute Myocardial Infarction: A Narrative Review. Cureus. 2022 Oct 30;14(10):e30868.
- Wilde AA, Antzelevitch C, Borggrefe M, et al; Study Group on the Molecular Basis of Arrhythmias of the European Society of Cardiology. Proposed diagnostic criteria for the Brugada syndrome. Eur Heart J. 2002 Nov;23(21):1648-54.
- Noori MAM, Fichadiya H, Jesani S, et al. A Rare yet Morbid Complication of Cocaine Use: Brugada Type 1 on Electrocardiogram. Cureus. 2022 Apr 20;14(4):e24309.
- Letsas KP, Weber R, Arentz T, et al. Brugada-type ECG pattern in patients treated with oral flecainide for lone atrial fibrillation: is there any clinical implication? Hellenic J Cardiol. 2009 Jul-Aug;50(4):338-9.
- Roomi SS, Ullah W, Abbas H, et al. Brugada syndrome unmasked by fever: a comprehensive review of literature. J Community Hosp Intern Med Perspect. 2020 Jun 14;10(3):224-228.
- Baranchuk A, Nguyen T, Ryu MH, et al. Brugada phenocopy: new terminology and proposed classification. Ann Noninvasive Electrocardiol. 2012 Oct;17(4):299-314.
- Genaro NR, Anselm DD, Cervino N, et al. Brugada phenocopy clinical reproducibility demonstrated by recurrent hypokalemia. Ann Noninvasive Electrocardiol. 2014 Jul;19(4):387-90.
- Zhang N, Liu T, Tse G, et al. Brugada phenocopy in a patient with acute pulmonary embolism presenting with recurrent syncope. Oxf Med Case Reports. 2017 May 30;2017(5):omx014.
- Xu G, Gottschalk BH, Pérez-Riera A, et al. Link between Brugada phenocopy and myocardial ischemia: Results from the International Registry on Brugada Phenocopy. Pacing Clin Electrophysiol. 2019 Jun;42(6):658-662.
- Papadakis M, Petzer E, Sharma S. Unmasking of the Brugada phenotype during exercise testing and its association with ventricular arrhythmia on the recovery phase. Heart. 2009 Dec;95(24):2022.
- de Oliveira Neto NR, de Oliveira WS, Mastrocola F, et al. Brugada phenocopy: Mechanisms, diagnosis, and implications. J Electrocardiol. 2019 Jul-Aug;55:45-50.
- Anselm DD, Gottschalk BH, Baranchuk A. Brugada Phenocopy Is an Important Differential Diagnosis in Patients with Type 1 Brugada ECG Patterns. Am J Med. 2015 Nov;128(11):e33.
Authors:
Jack Galla, B.S.
Medical Student
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL