January 2024 Issue
ISSN 2689-291X
ISSN 2689-291X
Cardiac Tamponade –
Respirophasic Right Ventricular Collapse!
Description
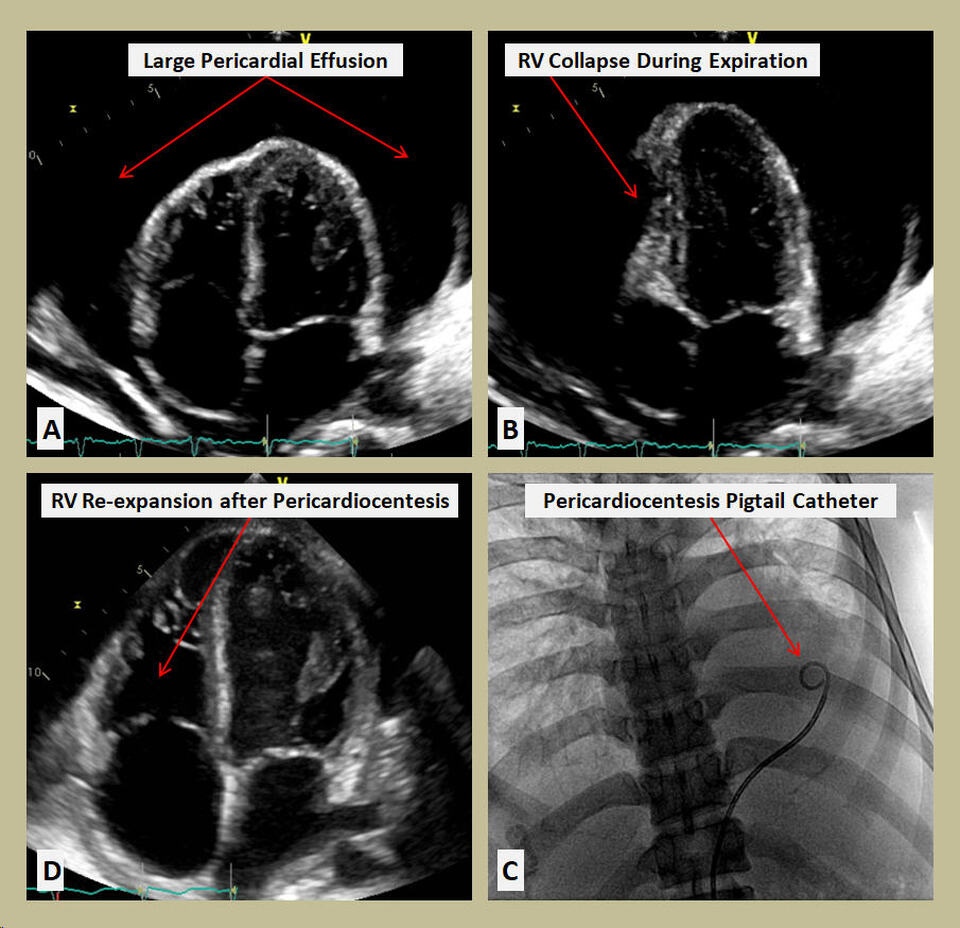
Figure A is a two-dimensional (2-D) transthoracic echocardiography (TTE) image in the apical 4-chamber view, showing a large pericardial effusion. In Figure B, the right ventricle (RV) is seen completely collapsed during expiration. Figure C demonstrates pericardiocentesis using a Pigtail catheter for drainage. In figure D, the RV is re-expanded following removal of pericardial fluid.
Discussion
The pericardium is a double walled pouch containing the heart and great vessel roots. The visceral and serosal layers of the pericardium form the pericardial space containing a physiologic amount of pericardial effusion, which provides lubrication and protection to the heart. Cardiac tamponade happens when a pericardial effusion increases and becomes large enough, or accumulates rapidly enough, to cause collapse of the right ventricle [1].
The most common causes of cardiac tamponade are pericarditis [2], postprocedural [3], and malignancy [4]. Less frequent causes include endocrine and autoimmune diseases [5, 6], trauma [7], and post myocardial infarction [8]. Infections or purulent pericarditis, especially in immunocompromised patients may progress to tamponade [9].
Adaptive stretching of the pericardium dictates the effects of tamponade. The pericardial space usually contains 50 mL of serous fluid. Rapid accumulation with an extra 100 mL of fluid can lead to critical cardiac compression. During inspiration, negative intrathoracic pressure augments right heart filling, while decreasing left heart filling leads to pulsus paradoxus (greater than 10 mmHg decrease in systolic blood pressure during inspiration). During expiration, however, the intrapericardial pressure overcomes the right ventricular pressure causing right ventricular collapse as shown above [10].
Symptoms of cardiac tamponade can include chest pain, tachypnea, dyspnea, dizziness and collapse. The classic physical findings of cardiac tamponade include Beck’s triad of hypotension, jugular venous distention, and muffled heart sounds. Additional clinical signs include tachycardia and pulsus paradoxus [11]. Electrocardiography can reveal decreased voltage with electrical alternans [12].
Several modalities can help with the diagnosis of cardiac tamponade, and multimodality imaging is often needed for optimal characterization of the etiology and pathophysiology of pericardial effusion [13]. Echocardiography, including point of care ultrasound, is most common and convenient initial test with well-established criteria to diagnose tamponade [14]. Cardiac computed tomography (CCT) and cardiac magnetic resonance imaging (CMR) may be used as second line imaging in cases of complex or loculated effusions or for further evaluation of extracardiac diseases [15, 16].
Treatment of cardiac tamponade is drainage with preferably needle paracentesis guided by imaging [17]. If there is intrapericardial bleeding or infection, surgical drainage with pericardiotomy or pericardial window may be needed [18]. For mild cases of tamponade without hemodynamic compromise, such as in idiopathic pericarditis or connective tissue/ inflammatory diseases, nonsteroidal anti-inflammatory drugs (NSAIDs) and colchicine, or steroids, may be used [19].
Conclusion
Cardiac tamponade is a highly morbid condition which requires a high index of suspicion and prompt testing with cardiac imaging, especially echocardiography, to establish the diagnosis and implement prompt life-saving therapies [20].
References
Authors:
Sangya Sharma, D.O.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Figure A is a two-dimensional (2-D) transthoracic echocardiography (TTE) image in the apical 4-chamber view, showing a large pericardial effusion. In Figure B, the right ventricle (RV) is seen completely collapsed during expiration. Figure C demonstrates pericardiocentesis using a Pigtail catheter for drainage. In figure D, the RV is re-expanded following removal of pericardial fluid.
Discussion
The pericardium is a double walled pouch containing the heart and great vessel roots. The visceral and serosal layers of the pericardium form the pericardial space containing a physiologic amount of pericardial effusion, which provides lubrication and protection to the heart. Cardiac tamponade happens when a pericardial effusion increases and becomes large enough, or accumulates rapidly enough, to cause collapse of the right ventricle [1].
The most common causes of cardiac tamponade are pericarditis [2], postprocedural [3], and malignancy [4]. Less frequent causes include endocrine and autoimmune diseases [5, 6], trauma [7], and post myocardial infarction [8]. Infections or purulent pericarditis, especially in immunocompromised patients may progress to tamponade [9].
Adaptive stretching of the pericardium dictates the effects of tamponade. The pericardial space usually contains 50 mL of serous fluid. Rapid accumulation with an extra 100 mL of fluid can lead to critical cardiac compression. During inspiration, negative intrathoracic pressure augments right heart filling, while decreasing left heart filling leads to pulsus paradoxus (greater than 10 mmHg decrease in systolic blood pressure during inspiration). During expiration, however, the intrapericardial pressure overcomes the right ventricular pressure causing right ventricular collapse as shown above [10].
Symptoms of cardiac tamponade can include chest pain, tachypnea, dyspnea, dizziness and collapse. The classic physical findings of cardiac tamponade include Beck’s triad of hypotension, jugular venous distention, and muffled heart sounds. Additional clinical signs include tachycardia and pulsus paradoxus [11]. Electrocardiography can reveal decreased voltage with electrical alternans [12].
Several modalities can help with the diagnosis of cardiac tamponade, and multimodality imaging is often needed for optimal characterization of the etiology and pathophysiology of pericardial effusion [13]. Echocardiography, including point of care ultrasound, is most common and convenient initial test with well-established criteria to diagnose tamponade [14]. Cardiac computed tomography (CCT) and cardiac magnetic resonance imaging (CMR) may be used as second line imaging in cases of complex or loculated effusions or for further evaluation of extracardiac diseases [15, 16].
Treatment of cardiac tamponade is drainage with preferably needle paracentesis guided by imaging [17]. If there is intrapericardial bleeding or infection, surgical drainage with pericardiotomy or pericardial window may be needed [18]. For mild cases of tamponade without hemodynamic compromise, such as in idiopathic pericarditis or connective tissue/ inflammatory diseases, nonsteroidal anti-inflammatory drugs (NSAIDs) and colchicine, or steroids, may be used [19].
Conclusion
Cardiac tamponade is a highly morbid condition which requires a high index of suspicion and prompt testing with cardiac imaging, especially echocardiography, to establish the diagnosis and implement prompt life-saving therapies [20].
References
- Adler Y, Ristić AD, Imazio M, Brucato A, Pankuweit S, Burazor I, Seferović PM, Oh JK. Cardiac tamponade. Nat Rev Dis Primers. 2023 Jul 20;9(1):36.
- Spodick DH. Pericarditis, pericardial effusion, cardiac tamponade, and constriction. Crit Care Clin. 1989 Jul;5(3):455-76.
- Alsenan AK, Al Dhneem HN, Alfandi HA, AlDahan HA, Almadan HM, AlSaif HH, Menezes RG. Iatrogenic Causes of Cardiac Tamponade Resulting From Surgical Procedures: An Overview. Cureus. 2023 Jan 14;15(1):e33773.
- Chahine J, Shekhar S, Mahalwar G, Imazio M, Collier P, Klein A. Pericardial Involvement in Cancer. Am J Cardiol. 2021 Apr 15;145:151-159.
- Chahine J, Jedeon Z, Chang KY, Jellis CL. Pericardial Manifestations of Thyroid Diseases. Curr Cardiol Rep. 2022 Aug;24(8):893-904.
- Kontzias A, Barkhodari A, Yao Q. Pericarditis in Systemic Rheumatologic Diseases. Curr Cardiol Rep. 2020 Sep 10;22(11):142.
- Fitzgerald M, Spencer J, Johnson F, Marasco S, Atkin C, Kossmann T. Definitive management of acute cardiac tamponade secondary to blunt trauma. Emerg Med Australas. 2005 Oct-Dec;17(5-6):494-9.
- Patil A, Singh N, Vigneshwaran S, Bharti S, Sudhakar S. Sudden Death Due to Cardiac Tamponade Secondary to Myocardial Infarction Ventricular Wall Rupture. Cureus. 2022 Oct 14;14(10):e30288.
- Williams D, Mulyala R, Riad M, Malozzi C, Omar B. Bacterial Pericarditis: Loculation Requiring Pericardiectomy! Cardiofel Newslet 2022. July; 5(7):21 – 23.
- Spodick DH. Pathophysiology of cardiac tamponade. Chest. 1998 May;113(5):1372-8.
- Imazio M, De Ferrari GM. Cardiac tamponade: an educational review. Eur Heart J Acute Cardiovasc Care. 2020 Jul 6:2048872620939341.
- Ingram D, Strecker-McGraw MK. Electrical Alternans. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
- Chetrit M, Xu B, Verma BR, Klein AL. Multimodality Imaging for the Assessment of Pericardial Diseases. Curr Cardiol Rep. 2019 Apr 16;21(5):41.
- Alerhand S, Carter JM. What echocardiographic findings suggest a pericardial effusion is causing tamponade? Am J Emerg Med. 2019 Feb;37(2):321-326.
- Restrepo CS, Lemos DF, Lemos JA, Velasquez E, Diethelm L, Ovella TA, Martinez S, Carrillo J, Moncada R, Klein JS. Imaging findings in cardiac tamponade with emphasis on CT. Radiographics. 2007 Nov-Dec;27(6):1595-610.
- Wang TKM, Ayoub C, Chetrit M, Kwon DH, Jellis CL, Cremer PC, Bolen MA, Flamm SD, Klein AL. Cardiac Magnetic Resonance Imaging Techniques and Applications for Pericardial Diseases. Circ Cardiovasc Imaging. 2022 Jul;15(7):e014283.
- Bafna KR, Kalra-Lall A, Gurajala RK, Karuppasamy K. Computed Tomography-Guided Pericardiocentesis: A Practical Guide. Curr Cardiol Rep. 2023 Nov;25(11):1433-1441.
- Oh NA, Hennecken C, Van den Eynde J, Doulamis IP, Avgerinos DV, Kampaktsis PN. Pericardiectomy and Pericardial Window for the Treatment of Pericardial Disease in the Contemporary Era. Curr Cardiol Rep. 2022 Nov;24(11):1619-1631.
- Imazio M, Adler Y. Treatment with aspirin, NSAID, corticosteroids, and colchicine in acute and recurrent pericarditis. Heart Fail Rev. 2013 May;18(3):355-60.
- Alerhand S, Adrian RJ, Long B, Avila J. Pericardial tamponade: A comprehensive emergency medicine and echocardiography review. Am J Emerg Med. 2022 Aug;58:159-174.
Authors:
Sangya Sharma, D.O.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL