July 2018 Issue
ISSN 2689-291X
ISSN 2689-291X
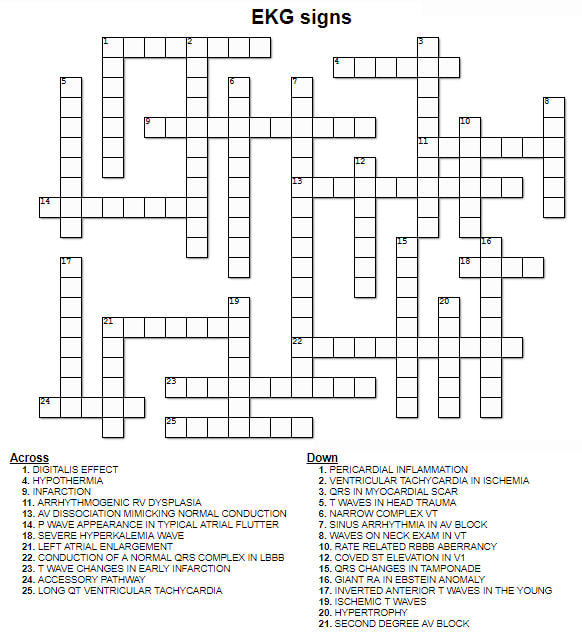
Crossword Puzzle
by Landai Nguyen, DO and Bassam Omar, MD, PhD
Journal Review
A Revascularization Conundrum:
Who Owns the Radial?
Abstract
A patient-level combined analysis of randomized, controlled trials was released on May 31st 2018 in the New England Journal of Medicine (1), comparing radial artery grafts (RAG) to saphenous vein grafts (SVG) in patients who underwent coronary artery bypass grafting (CABG). Primary outcome included major adverse cardiac events (MACE) at follow up, including myocardial infarction (MI), repeat revascularization, and death.
Six trials were analyzed, consisting of 1305 patients; the mean follow up time was 60 ± 30 months. A total of 534 patients received RAG, and 502 patients received SVG.
Patient characteristics:
Results
Conclusion
Arterial grafts have been shown to be superior to vein grafts in multiple observational studies, in terms of patency, at follow-up; it remains unclear, however, whether this impacts mortality. Greater than 90% of patients receive only one arterial graft at the time of CABG in the United States. More randomized trials are needed to assess for any mortality benefit of radial artery grafts over saphenous vein grafts.
Conundrum
Cardiac catheterizations and percutaneous coronary interventions (PCI) are increasingly performed using radial artery access to reduce vascular complications and hasten recovery. Patients are more often referred to CABG following multiple PCIs, many of which may have utilized one or both radial arteries. The suitability of a radial artery as a conduit in CABG following trans-radial catheterization has been called in question due to damage and hyperplasia leading to lower patency as a bypass graft (2). In this era of flourishing radial catheterizations we have to step back and ask: who owns the radial? Should interventionalists give up the convenience of the trans-radial approach to allow surgeons to safely use the radial as a superior conduit? Further research is needed to identify ways to limit radial artery damage during trans-radial catheterization.
References
Authors
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
A patient-level combined analysis of randomized, controlled trials was released on May 31st 2018 in the New England Journal of Medicine (1), comparing radial artery grafts (RAG) to saphenous vein grafts (SVG) in patients who underwent coronary artery bypass grafting (CABG). Primary outcome included major adverse cardiac events (MACE) at follow up, including myocardial infarction (MI), repeat revascularization, and death.
Six trials were analyzed, consisting of 1305 patients; the mean follow up time was 60 ± 30 months. A total of 534 patients received RAG, and 502 patients received SVG.
Patient characteristics:
- Similar in terms of age, gender, diabetes prevalence, presence of LV dysfunction (EF < 35%) and renal insufficiency in both groups.
- The left circumflex artery was the target vessel in 75%, while the right coronary artery was the target vessel in 25% of the cases.
- 19 graft occlusion events per 1000 patient – year in RAG
- 46 graft occlusion events per 1000 patient – year in SVG
Results
- Lower incidence of death, MI, and repeat revascularization in the radial artery group (25 vs 39 events per 1000 patient – years) when compared to saphenous vein grafts.
- No significant difference in death from any cause (15 vs 17 events per 1000 patient-years).
- Improved MACE, in women, < 75 year old, and without renal insufficiency.
- Lower risk of RAG occlusion in women.
Conclusion
Arterial grafts have been shown to be superior to vein grafts in multiple observational studies, in terms of patency, at follow-up; it remains unclear, however, whether this impacts mortality. Greater than 90% of patients receive only one arterial graft at the time of CABG in the United States. More randomized trials are needed to assess for any mortality benefit of radial artery grafts over saphenous vein grafts.
Conundrum
Cardiac catheterizations and percutaneous coronary interventions (PCI) are increasingly performed using radial artery access to reduce vascular complications and hasten recovery. Patients are more often referred to CABG following multiple PCIs, many of which may have utilized one or both radial arteries. The suitability of a radial artery as a conduit in CABG following trans-radial catheterization has been called in question due to damage and hyperplasia leading to lower patency as a bypass graft (2). In this era of flourishing radial catheterizations we have to step back and ask: who owns the radial? Should interventionalists give up the convenience of the trans-radial approach to allow surgeons to safely use the radial as a superior conduit? Further research is needed to identify ways to limit radial artery damage during trans-radial catheterization.
References
- Gaudino, M., Benedetto, U., Fremes, S. et al. “Radial Artery or Saphenous Vein Grafts in Coronary Artery Bypass Surgery.” New England Journal of Medicine. Vol. 378. No. 22. May 31 2018.
- Mounsey CA, Mawhinney JA, Werner RS, Taggart DP. “Does Previous Transradial Catheterization Preclude Use of the Radial Artery as a Conduit in Coronary Artery Bypass Surgery?” Circulation. 2016 Aug 30;134(9):681-8.
Authors
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
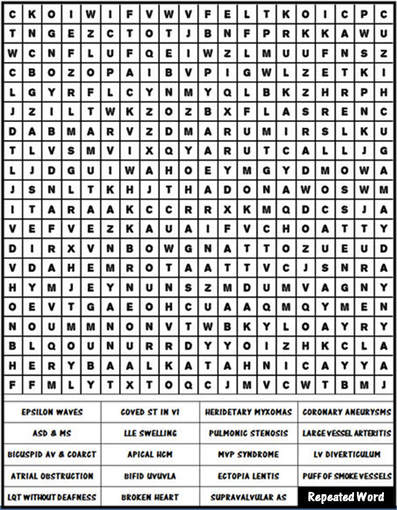
Find a Condition
by Sarina Sachdev, MD and Bassam Omar, MD, PhD
Journal Review
Carvedilol: A Promising Tool in the Meager
Armamentarium of the Cardio-Oncologist!
Abstract
The CECCY Trial (Carvedilol for Prevention of Chemotherapy-Related Cardiotoxicity) is a recently published prospective, randomized, double-blind, placebo-controlled study which examined the role of carvedilol in the prevention of chemotherapy-related cardiotoxicity (1). This was specifically defined in this study as a decline in left ventricular ejection fraction (LVEF) of 10% at 6 months after start of chemotherapy. Other end-points examined were carvedilol’s effect on cardiac troponin, B-type natriuretic peptide, and diastolic dysfunction, among other measurable echocardiographic parameters.
Patients were eligible if they were receiving anthracycline (ANT) chemotherapy for HER2-negative breast cancer and had a normal LVEF prior to chemotherapy. The study investigators identified and randomized 200 such patients to receive carvedilol or placebo throughout the duration of chemotherapy (which included cyclophosphamide, doxorubicin at a total cumulative dose of 240 mg/m2, and paclitaxel).
The CECCY Trial is one of a few randomized, prospective trials studying the effects of beta blockers, specifically carvedilol, on chemotherapy induced cardiotoxicity. Previous studies evaluating beta blockers for the prevention of chemotherapy-related cardiotoxicity have been somewhat controversial because of design limitations (2 – 4). The more recent PRADA trial (5), however, was well designed to address the primary prevention hypothesis. It was a double-blind, placebo controlled trial with a 2 x 2 factorial randomized design. Breast cancer patients enrolled also received ANT but may also have received trastuzumab and/or radiation. Patients receiving the latter were excluded in the CECCY trial. Subjects were assigned metoprolol succinate, candesartan, or placebo. There was no effect on LVEF in the metoprolol group. However, data favored the use of candesartan. The CECCY investigators were able to compile a larger patient population and focus on one chemotherapeutic agent and one therapeutic intervention. They hypothesized that the use of a different beta blocker with different pharmacologic properties than metoprolol succinate could succeed in primary prevention of chemotherapy related cardiomyopathy (CrCM).
Results
A drop in LVEF of 10% occurred in 14 patients receiving carvedilol and 13 patients receiving placebo (p = 1.0). For the majority of patients with a decrease in LVEF in each group, their LVEF did not fall outside the normal range. There was one patient in each group with an LVEF drop of more than 10%, to a level of < 55%. No significant differences in change of LVEF were noted. There was, however, a significant difference between groups in troponin I (TnI) levels over time (p = 0.003). The carvedilol group had lower TnI levels compared to placebo. Also, a lower incidence of diastolic dysfunction was noted in the carvedilol group (p = 0.039). Although nonsignificant, there was a trend toward a less pronounced increase in left ventricular end-diastolic diameter in the carvedilol group (44.1 ± 3.6 mm to 45.2 ± 3.2 mm; 2.5% increase) compared with the placebo group (44.9 ± 3.6 mm to 46.4 ± 4.0 mm; 3.3% increase; p = 0.057).
Therefore, although after 6-month therapy with carvedilol alongside chemotherapy, the addition of carvedilol did not significantly impact the LVEF, more importantly, there was a statistical significance of the use of carvedilol leading to lower troponin levels and less diastolic dysfunction as compared to placebo.
Conclusion
While this study did not prove carvedilol to be successful in primary prevention of ANT related cardiomyopathy and LVEF decline, all was not lost. The study’s secondary end points provided some insight into potential benefits of carvedilol and avenues for further research. The study concluded that carvedilol may delay the onset of cardiac myocyte injury (significantly lower levels of cardiac TnI levels compared to placebo) and possibly attenuate adverse cardiac remodeling (lesser degree of LV dilation and fewer patients with diastolic dysfunction).
There were no serious adverse effects noted from the addition of carvedilol, thereby posing the question, whether the slight benefit outweighs any minimal risk of the addition of beta blockers in this patient group. Another interesting thought is the effect of carvedilol past the 6-month period used in this study. Anthracyclines can cause both early and late dose cardiotoxicity. Though there was no benefit of carvedilol in the early phase of anthracycline exposure, it would be interesting to see if there are any significant long-term benefits of carvedilol beyond the completion of the chemotherapy.
Ultimately, this study identifies other potential research targets to be explored as well as the need for larger studies to evaluate the effects of other pharmacologic interventions in the arena of primary prevention of chemotherapy induced cardiotoxicity.
Clinical Implications
Survival rates in cancer patients have increased steadily over the last few decades (6). This is primarily due to rapid advancements in cancer therapies. However, many chemotherapeutic agents are invariably cardiotoxic. Cardiovascular complications of cancer treatment portend significantly poorer outcomes with worsened morbidity and mortality in these patients. One of the more commonly recognized cardiotoxicities is the development of CrCM and heart failure (HF). ANT use is very common among female patients undergoing treatment for breast cancer. ANTs are associated with early and late dose-related cardiotoxicity, primarily HF (7 – 9). This study examined the effects of carvedilol on prevention of CrCM. Cardiologists who are referred a patient with HFrEF secondary to CrCM will likely reach for routine guideline directed therapy for HF. Likely, they will start with an angiotensin converting enzyme inhibitor (ACE-I), beta blocker (BB), or both in attempt to prevent worsening of cardiac function and HF, and hopefully improve LVEF. Unfortunately, with many CrCMs, the myocardial damage is often not appreciably reversible. This is often the case with ANT exposure. Identifying ways to prevent cardiotoxicity has been the focus of much research including pharmacotherapy and imaging techniques. Despite the significant insights gained from many recent studies, there remains a major gap in our understanding of the mechanisms and ability to alter this debilitating consequence of chemotherapy.
References
Authors
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
The CECCY Trial (Carvedilol for Prevention of Chemotherapy-Related Cardiotoxicity) is a recently published prospective, randomized, double-blind, placebo-controlled study which examined the role of carvedilol in the prevention of chemotherapy-related cardiotoxicity (1). This was specifically defined in this study as a decline in left ventricular ejection fraction (LVEF) of 10% at 6 months after start of chemotherapy. Other end-points examined were carvedilol’s effect on cardiac troponin, B-type natriuretic peptide, and diastolic dysfunction, among other measurable echocardiographic parameters.
Patients were eligible if they were receiving anthracycline (ANT) chemotherapy for HER2-negative breast cancer and had a normal LVEF prior to chemotherapy. The study investigators identified and randomized 200 such patients to receive carvedilol or placebo throughout the duration of chemotherapy (which included cyclophosphamide, doxorubicin at a total cumulative dose of 240 mg/m2, and paclitaxel).
The CECCY Trial is one of a few randomized, prospective trials studying the effects of beta blockers, specifically carvedilol, on chemotherapy induced cardiotoxicity. Previous studies evaluating beta blockers for the prevention of chemotherapy-related cardiotoxicity have been somewhat controversial because of design limitations (2 – 4). The more recent PRADA trial (5), however, was well designed to address the primary prevention hypothesis. It was a double-blind, placebo controlled trial with a 2 x 2 factorial randomized design. Breast cancer patients enrolled also received ANT but may also have received trastuzumab and/or radiation. Patients receiving the latter were excluded in the CECCY trial. Subjects were assigned metoprolol succinate, candesartan, or placebo. There was no effect on LVEF in the metoprolol group. However, data favored the use of candesartan. The CECCY investigators were able to compile a larger patient population and focus on one chemotherapeutic agent and one therapeutic intervention. They hypothesized that the use of a different beta blocker with different pharmacologic properties than metoprolol succinate could succeed in primary prevention of chemotherapy related cardiomyopathy (CrCM).
Results
A drop in LVEF of 10% occurred in 14 patients receiving carvedilol and 13 patients receiving placebo (p = 1.0). For the majority of patients with a decrease in LVEF in each group, their LVEF did not fall outside the normal range. There was one patient in each group with an LVEF drop of more than 10%, to a level of < 55%. No significant differences in change of LVEF were noted. There was, however, a significant difference between groups in troponin I (TnI) levels over time (p = 0.003). The carvedilol group had lower TnI levels compared to placebo. Also, a lower incidence of diastolic dysfunction was noted in the carvedilol group (p = 0.039). Although nonsignificant, there was a trend toward a less pronounced increase in left ventricular end-diastolic diameter in the carvedilol group (44.1 ± 3.6 mm to 45.2 ± 3.2 mm; 2.5% increase) compared with the placebo group (44.9 ± 3.6 mm to 46.4 ± 4.0 mm; 3.3% increase; p = 0.057).
Therefore, although after 6-month therapy with carvedilol alongside chemotherapy, the addition of carvedilol did not significantly impact the LVEF, more importantly, there was a statistical significance of the use of carvedilol leading to lower troponin levels and less diastolic dysfunction as compared to placebo.
Conclusion
While this study did not prove carvedilol to be successful in primary prevention of ANT related cardiomyopathy and LVEF decline, all was not lost. The study’s secondary end points provided some insight into potential benefits of carvedilol and avenues for further research. The study concluded that carvedilol may delay the onset of cardiac myocyte injury (significantly lower levels of cardiac TnI levels compared to placebo) and possibly attenuate adverse cardiac remodeling (lesser degree of LV dilation and fewer patients with diastolic dysfunction).
There were no serious adverse effects noted from the addition of carvedilol, thereby posing the question, whether the slight benefit outweighs any minimal risk of the addition of beta blockers in this patient group. Another interesting thought is the effect of carvedilol past the 6-month period used in this study. Anthracyclines can cause both early and late dose cardiotoxicity. Though there was no benefit of carvedilol in the early phase of anthracycline exposure, it would be interesting to see if there are any significant long-term benefits of carvedilol beyond the completion of the chemotherapy.
Ultimately, this study identifies other potential research targets to be explored as well as the need for larger studies to evaluate the effects of other pharmacologic interventions in the arena of primary prevention of chemotherapy induced cardiotoxicity.
Clinical Implications
Survival rates in cancer patients have increased steadily over the last few decades (6). This is primarily due to rapid advancements in cancer therapies. However, many chemotherapeutic agents are invariably cardiotoxic. Cardiovascular complications of cancer treatment portend significantly poorer outcomes with worsened morbidity and mortality in these patients. One of the more commonly recognized cardiotoxicities is the development of CrCM and heart failure (HF). ANT use is very common among female patients undergoing treatment for breast cancer. ANTs are associated with early and late dose-related cardiotoxicity, primarily HF (7 – 9). This study examined the effects of carvedilol on prevention of CrCM. Cardiologists who are referred a patient with HFrEF secondary to CrCM will likely reach for routine guideline directed therapy for HF. Likely, they will start with an angiotensin converting enzyme inhibitor (ACE-I), beta blocker (BB), or both in attempt to prevent worsening of cardiac function and HF, and hopefully improve LVEF. Unfortunately, with many CrCMs, the myocardial damage is often not appreciably reversible. This is often the case with ANT exposure. Identifying ways to prevent cardiotoxicity has been the focus of much research including pharmacotherapy and imaging techniques. Despite the significant insights gained from many recent studies, there remains a major gap in our understanding of the mechanisms and ability to alter this debilitating consequence of chemotherapy.
References
- Avila MS, Ayub-Ferreira SM, de Barros Wanderley MR Jr et al. Carvedilol for prevention of chemotherapy-related cardiotoxicity: the CECCY trial. J Am Coll Cardiol 2018;71:2281-90
- Seicean S., Seicean A., Alan N. et al. Cardioprotective effect of β-adrenoceptor blockade in patients with breast cancer undergoing chemotherapy: follow-up study of heart failure. Circ Heart Fail 2013;6:420–426
- Bosch X., Rovira M., Sitges M. et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies). J Am Coll Cardiol 2013;61:2355–2362
- Kalay N., Basar E., Ozdogru I. et al. Kalay N., Basar E., Ozdogru I. et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J Am Coll Cardiol 2006;48:2258–2262
- Gulati G., Heck S.L., Ree A.H., et al. Prevention of Cardiac Dysfunction During Adjuvant Breast Cancer Therapy (PRADA): a 2 × 2 factorial, randomized, placebo-controlled, double-blind clinical trial of candesartan and metoprolol. Eur Heart J 2016;37:1671–1680
- Bluethmann S.M., Mariotto A.B., Rowland J.H. Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomark Prev 2016;25:1029–1036
- Suter T.M., Ewer M.S. Cancer drugs and the heart: importance and management. Eur Heart J 2013;34:1102–1111
- Valachis A., Nilsson C. Cardiac risk in the treatment of breast cancer: assessment and management. Breast Cancer (Dove Med Press) 2015;7:21–35
- Henriksen P.A. Anthracycline cardiotoxicity: an update on mechanisms, monitoring and prevention. Heart 2018;104:971-977
Authors
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL