July 2020 Issue
ISSN 2689-291X
ISSN 2689-291X
Left Atrial Myxoma.. The Incredible Bulk!
Description
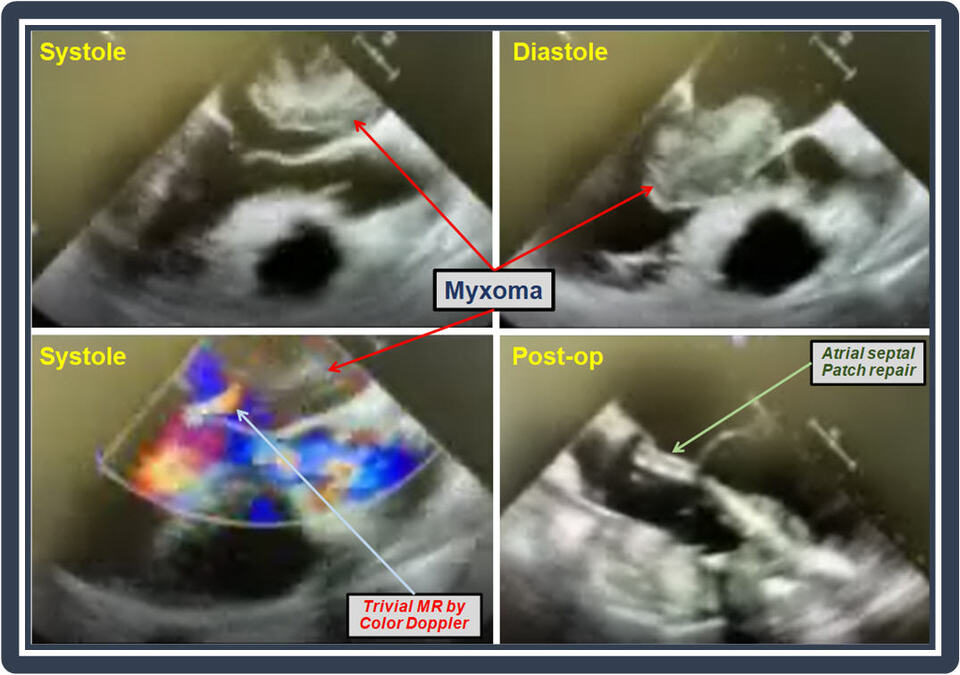
The above images and the accompanying video clips reveal multiple transesophageal echocardiography views of a large left atrial myxoma attached to the interatrial septum which is prolapsing into the mitral valve in diastole causing obstruction. Post-operative images are shown, which reveal absence of the myxoma and patch repair of the inter-atrial septum.
Discussion:
Primary cardiac tumors are very rare with an average incidence of 0.02% (0.002% – 0.2%) in unselected autopsy patients [1, 2]. Greater than 75% of PCTs are benign neoplasms; of these, approximately 50% are myxomas [3]. Most cardiac myxoma cases are reported in the fourth to seventh decade of life and are more prevalent in females. Nevertheless, cases are seen in all age and gender groups [4].
Clinical manifestations are dependent on the location and size of the myxoma [5], with unusual manifestation often seen in uncommon tumor locations [6]. Approximately 75% of cardiac myxomas develop in the left atrium, 23% in the right atrium, and the remainder in the ventricles [7]. The three most common causes of symptoms of a cardiac myxoma are hemodynamic changes [8], systemic embolism [9], and cytokine release leading to constitutional symptoms [10]. Commonly observed symptoms and signs are dyspnea, orthopnea, pulmonary edema, cough, and fatigue [11, 12]. Symptoms such as fever and weight loss are seen in 30% of patients, mimicking endocarditis [13]. Additionally, elevations in erythrocyte sedimentation rate [14], globulin levels [15], or C-reactive protein levels [16] are present in up to 35% of patients.
Initial assessment includes taking a detailed clinical history and having a high index of suspicious for cardiac myxoma as it can mimic many systemic disease presentations [17]. Physical examination signs such as cannon “A” wave have been reported in right atrial myxomas [18]. Cardiac auscultation is also crucial for the pathognomonic “tumor plop”, a mid to late diastolic sound [19]. Initial testing is typically conducted using transthoracic or transesophageal echocardiography [20]. Other imaging modalities such as cardiac magnetic resonance (CMR) [21], contrast-enhanced cardiac computed tomography (CCT) [22] may also be helpful in providing more information on the tumor type and location. Multimodality imaging is often utilized to characterize the location, attachments and vascularity of a cardiac myxoma in preparation for surgical intervention [23].
The standard treatment for cardiac myxoma is surgical resection, with low reported complications and good surgical outcomes [24]. When the site of attachment is the atrial septum, this is usually resected, necessitating concomitant atrial septal defect repair (as in images shown above), with successful less invasive thoracoscopic [25] and robotic [26] surgical procedures reported. Rarely, damage to the mitral valve [27] or tricuspid valve [28] necessitates simultaneous valve replacement.
Conclusion:
Cardiac myxomas are rare benign but often bulky tumors with variable clinical presentations which can mimic many cardiac and systemic diseases based on their size, friability and inflammatory potential. Specific physical examination and cardiac auscultation signs can help in the diagnosis. Cardiac myxomas can be familial, part of the Carney complex [29] which may be recurrent [30] or sporadic. Diagnosis often requires multimodality imaging and treatment is usually surgical, requiring a heart-team multidisciplinary approach for optimal outcomes.
References:
Authors:
Saad Awan, B.S.
Medical Student
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Umer Awan, M.D.
Staff Cardiologist
Iowa Methodist Medical Center. The Iowa Clinic, P.C.
Des Moines, IA
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The above images and the accompanying video clips reveal multiple transesophageal echocardiography views of a large left atrial myxoma attached to the interatrial septum which is prolapsing into the mitral valve in diastole causing obstruction. Post-operative images are shown, which reveal absence of the myxoma and patch repair of the inter-atrial septum.
Discussion:
Primary cardiac tumors are very rare with an average incidence of 0.02% (0.002% – 0.2%) in unselected autopsy patients [1, 2]. Greater than 75% of PCTs are benign neoplasms; of these, approximately 50% are myxomas [3]. Most cardiac myxoma cases are reported in the fourth to seventh decade of life and are more prevalent in females. Nevertheless, cases are seen in all age and gender groups [4].
Clinical manifestations are dependent on the location and size of the myxoma [5], with unusual manifestation often seen in uncommon tumor locations [6]. Approximately 75% of cardiac myxomas develop in the left atrium, 23% in the right atrium, and the remainder in the ventricles [7]. The three most common causes of symptoms of a cardiac myxoma are hemodynamic changes [8], systemic embolism [9], and cytokine release leading to constitutional symptoms [10]. Commonly observed symptoms and signs are dyspnea, orthopnea, pulmonary edema, cough, and fatigue [11, 12]. Symptoms such as fever and weight loss are seen in 30% of patients, mimicking endocarditis [13]. Additionally, elevations in erythrocyte sedimentation rate [14], globulin levels [15], or C-reactive protein levels [16] are present in up to 35% of patients.
Initial assessment includes taking a detailed clinical history and having a high index of suspicious for cardiac myxoma as it can mimic many systemic disease presentations [17]. Physical examination signs such as cannon “A” wave have been reported in right atrial myxomas [18]. Cardiac auscultation is also crucial for the pathognomonic “tumor plop”, a mid to late diastolic sound [19]. Initial testing is typically conducted using transthoracic or transesophageal echocardiography [20]. Other imaging modalities such as cardiac magnetic resonance (CMR) [21], contrast-enhanced cardiac computed tomography (CCT) [22] may also be helpful in providing more information on the tumor type and location. Multimodality imaging is often utilized to characterize the location, attachments and vascularity of a cardiac myxoma in preparation for surgical intervention [23].
The standard treatment for cardiac myxoma is surgical resection, with low reported complications and good surgical outcomes [24]. When the site of attachment is the atrial septum, this is usually resected, necessitating concomitant atrial septal defect repair (as in images shown above), with successful less invasive thoracoscopic [25] and robotic [26] surgical procedures reported. Rarely, damage to the mitral valve [27] or tricuspid valve [28] necessitates simultaneous valve replacement.
Conclusion:
Cardiac myxomas are rare benign but often bulky tumors with variable clinical presentations which can mimic many cardiac and systemic diseases based on their size, friability and inflammatory potential. Specific physical examination and cardiac auscultation signs can help in the diagnosis. Cardiac myxomas can be familial, part of the Carney complex [29] which may be recurrent [30] or sporadic. Diagnosis often requires multimodality imaging and treatment is usually surgical, requiring a heart-team multidisciplinary approach for optimal outcomes.
References:
- Reynen K. Frequency of primary tumors of the heart. Am J Cardiol. 1996; 77(1):107.
- Reynen K. Cardiac myxomas. N Engl J Med. 1995; 333(24):1610-1617.
- Yu K, Liu Y, Wang H, et al. Epidemiological and pathological characteristics of cardiac tumors: a clinical study of 242 cases. Interact Cardiovasc Thorac Surg. 2007;6(5):636-639.
- Grebenc ML, Rosado-de-Christenson ML, Green CE, et al. Cardiac myxoma: imaging features in 83 patients. Radiographics. 2002;22(3):673-689.
- Garcia-Carretero R, Vela BB, Martínez-Quesada G, et al. Demographic and clinical features of atrial myxomas: A case series analysis. Acute Card Care. 2016;18(3):65-69.
- Yuan SM, Yan SL, Wu N. Unusual aspects of cardiac myxoma. Anatol J Cardiol. 2017;17(3):241-247.
- Markel ML, Waller BF, Armstrong WF. Cardiac myxoma. A review. Medicine (Baltimore). 1987;66(2):114-125.
- Sung RJ, Ghahramani AR, Mallon SM, et al. Hemodynamic features of prolapsing and nonprolapsing left atrial myxoma. Circulation. 1975;51(2):342-349.
- Zhang RD, Zeng ZH, Zheng JY, et al. Left atrial myxoma complicated with multi-system embolization. J Cardiothorac Surg. 2017;12(1):76.
- Wiedermann CJ, Reinisch N, Fischer-Colbrie R, et al. Proinflammatory cytokines in cardiac myxomas. J Intern Med. 1992;232(3):263-265.
- Karabinis A, Samanidis G, Khoury M, et al. Clinical presentation and treatment of cardiac myxoma in 153 patients. Medicine (Baltimore). 2018;97(37):e12397.
- Cohen R, Singh G, Mena D, Garcia CA, Loarte P, Mirrer B. Atrial Myxoma: A Case Presentation and Review. Cardiol Res. 2012;3(1):41-44.
- Fitzgerald GP, Coughlan JJ, Satti Z, et al. Atrial myxoma presenting as infective endocarditis. BMJ Case Rep. 2018;2018: bcr2017223656.
- Ekström M, Svenarud P. Atrial myxoma: a rare but well-described cause of increased erythrocyte sedimentation rate and anaemia. BMJ Case Rep. 2015;2015:bcr2015209820.
- Jourdan M, Bataille R, Seguin J, et al. Constitutive production of interleukin-6 and immunologic features in cardiac myxomas. Arthritis Rheum. 1990;33(3):398-402.
- Cho J, Quach S, Reed J, et al. Case report: left atrial Myxoma causing elevated C-reactive protein, fatigue and fever, with literature review. BMC Cardiovasc Disord. 2020;20(1):119.
- Kalra DK, Hemu M, Kyung S, et al. Atrial myxoma-the Great Masquerader. QJM. 2019;112(5):363-364.
- Wakefield BJ, Alfirevic A. Right Atrial Myxoma with Cannon A Waves. Anesthesiology. 2018;128(1):143.
- Kolluru A, Desai D, Cohen GI. The etiology of atrial myxoma tumor plop. J Am Coll Cardiol. 2011;57(21):e371.
- Sachdev S, Nguyen L, Tahir H, et al. Cardiac Myxoma.. So Common, Yet So Rare! Cardiofel Newslet 2019 January; 2(1): 1-2.
- Abbas A, Garfath-Cox KA, Brown IW, Shambrook JS, Peebles CR, Harden SP. Cardiac MR assessment of cardiac myxomas. Br J Radiol. 2015;88(1045):20140599.
- Haji K, Nasis A. Radiological characteristics of atrial myxoma in Cardiac Computed Tomography. J Cardiovasc Comput Tomogr. 2017;11(3):234-236.
- Colin GC, Gerber BL, Amzulescu M, Bogaert J. Cardiac myxoma: a contemporary multimodality imaging review. Int J Cardiovasc Imaging. 2018;34(11):1789-1808.
- Abu Abeeleh M, Saleh S, Alhaddad E, et al. Cardiac myxoma: clinical characteristics, surgical intervention, intra-operative challenges and outcome. Perfusion. 2017;32(8):686-690.
- Deng L, Zhang GW, Liu ZH, Meng WX, Liu HY. Totally thoracoscopic surgery for atrial myxomas resection and atrial septal defect repair. Eur Rev Med Pharmacol Sci. 2017;21(3):569-575.
- Gao C, Yang M, Wang G, Wang J. Totally robotic resection of myxoma and atrial septal defect repair. Interact Cardiovasc Thorac Surg. 2008;7(6):947-950.
- Bozer AY, Kural T, Yurdakul Y, Aytac A. Left atrial myxoma causing mitral insufficiency. Report of a case treated with mitral valve replacement. J Cardiovasc Surg (Torino). 1975;16(5):535-537.
- Hattori M, Matsumura Y, Yamaki F. Myxoma Originating From the Tricuspid Annulus Requiring Annular Reconstruction and Valve Replacement;Report of a Case. [in Japanese]. Kyobu Geka. 2016; 69(7):552-555.
- Wei K, Guo HW, Fan SY, Sun XG, Hu SS. Clinical features and surgical results of cardiac myxoma in Carney complex. J Card Surg. 2019;34(1):14-19.
- Wang L, Wang Q, Zhou Y, et al. Recurrent left atrial myxoma in Carney complex: A case report of a familial pedigree. Medicine (Baltimore). 2018;97(12):e0247.
Authors:
Saad Awan, B.S.
Medical Student
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Umer Awan, M.D.
Staff Cardiologist
Iowa Methodist Medical Center. The Iowa Clinic, P.C.
Des Moines, IA
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
COVID-19: Medical Education Transformation
Prelude
The emergence of the novel coronavirus (COVID-19) pandemic has instigated a global emergency that poses unprecedented challenges to all functions of modern society, especially business and education [1]. While online education [2] was a plausible alternative to in-person classes for many schools and institutes of higher education, such an option may not fulfill all the requirements of medical education, where outcomes are reliant on team-based work during a delicate timeline. Students are already struggling to mitigate the pandemic’s delays and disruptions to their career development while faculty is striving to accommodate changes without taking away from their students’ education [3].
Major Transformation
Modern medical education promotes a holistic and collaborative teaching environment where students learn vital interpersonal and leadership skills. Additionally, today’s medical schools emphasize the importance of hospital-based early clinical exposure during pre-clerkship years. The COVID-19 pandemic is causing major disturbances to classroom and hospital training environments, placing these foundations for a successful medical education at great risk [4]. Social distancing, as recommended by the Centers for Disease Control and Prevention (CDC), remains a powerful measure to retard the pandemic’s growth [5]. Therefore, one swift change many medical schools adopted was cancellation of in-person classes and moving to pre-recorded or live-streamed lectures [6]. The loss of a group experience and in-person feedback offered in a classroom setting may eventually be unfavorable to student learning, especially for those who thrive in an in-person learning environment [7]. In order to remedy this learning gap, medical schools have also turned to online platforms like Zoom, which allow interactive group discussions [8]. While the movement to online curricula does accommodate social distancing guidelines and may satisfy some of the requirements for undergraduate medical education [9], its outcomes and effectiveness are unclear and may potentially be suboptimal in graduate medical education [10], where a greater degree of hands-on experience is crucial to learning many patient care skills.
The COVID-19 pandemic continues to have a negative impact on student learning during their clerkship years. Many schools have cancelled clinical clerkships in an effort to limit personal interaction in the hospital, conserve personal protective equipment, and reduce the risk of exposure for their students [11]. Other factors that limit student clinical participation in the clinical environment include the shortages of COVID-19 testing [12], cancelation of elective surgical procedures [13], and increased use of telehealth [14]. This presents a challenge to providing students with authentic patient experiences [15]. Educators are increasingly moving clinical experiences to an online format, deferring clinical time to a later date, or incorporating virtual case studies in education [16]. Current options remain limited and are forcing several revolutionary changes to the traditional tools of medical education [17], calling for innovative novel strategies to address the issue [18]. Ongoing re-evaluation of the pandemic’s impact on clinical education is necessary so medical schools can decide on effective and sustainable policies [19].
Graduate medical education has also seen many challenges and innovations as a result of the pandemic [20]. Residents and fellows are already seeing a change in patient relationship as the pandemic evolves, with reliance on technology to fill in the gaps in traditional bedside teaching [21]. Fellowship training overall may have a greater requirement for procedural competencies which are difficult to accommodate because of the COVID-19 pandemic. The exponential numbers of COVID-19 cases in certain states has called for deployment of fellow trainees, especially in cardiology [22], to care for such patients, as allowed by the Accreditation Commission on Graduate Medical Education (ACGME), which understandably takes away from the time for fellowship training. Several major medical and surgical societies, including the American College of Cardiology (ACC), recommended limiting elective surgeries and procedures, including cardiac procedures, and curtailing trainee role in urgent procedures involving COVID-19 confirmed or suspect patients in order to reduce infection exposure [23]. Moreover, the role of interventional cardiac procedures in the care of COVID-19 patients has also diminished with greater reliance on non-interventional treatments [24]. Such limitations have placed tremendous strain on fellowships, especially in interventional cardiology, requiring tailored training strategies to provide adequate procedural competencies [25]. The American Society of Echocardiography (ASE) provided a guidance statement for the provision of echocardiography services during the COVID-19 pandemic, which would be expected to limit the number of echocardiography procedures and likely impact fellowship training in cardiology as well [26]. The extent to which all these unprecedented constraints will impact the quality of education in cardiology and other fellowship training remains unknown and would need careful evaluation and mitigation [27].
The Future
The COVID-19 pandemic has unequivocally resulted in major transformations to the undergraduate and graduate medical education, calling for timely innovations and modernization. While all aspects of education have been affected by the pandemic, the impact has been greatest on advanced training in cardiology and procedural competencies in the US and other countries [28]. This has created tremendous angst amongst training programs as nontraditional and less-proven methods of education had to be adopted. Reliance on less sophisticated tool for diagnosis may provide an opportunity to revive the role of the stethoscope in medical training in general and cardiology training in particular [29]. However, the cardiology field has come very far in providing high tech diagnostic and therapeutic procedures proven to impact morbidity and mortality, which require rigorous training according to strict guidelines. The expectation is that future generations of cardiologists will not only be competent in such procedures, but also be able to provide further innovations which will continue to improve patient outcomes. Development of procedural competencies may require increased reliance on robust simulation tools to prepare trainees and reduce their encounter time with real patients [30]. Humanity has suffered unfathomable distress from the pandemic at multiple levels, most importantly education; the response has been substantial concerted crisis-driven innovations which will hopefully positively guide future generations.
References:
Authors:
Saad Awan, B.S.
Medical Student
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The emergence of the novel coronavirus (COVID-19) pandemic has instigated a global emergency that poses unprecedented challenges to all functions of modern society, especially business and education [1]. While online education [2] was a plausible alternative to in-person classes for many schools and institutes of higher education, such an option may not fulfill all the requirements of medical education, where outcomes are reliant on team-based work during a delicate timeline. Students are already struggling to mitigate the pandemic’s delays and disruptions to their career development while faculty is striving to accommodate changes without taking away from their students’ education [3].
Major Transformation
Modern medical education promotes a holistic and collaborative teaching environment where students learn vital interpersonal and leadership skills. Additionally, today’s medical schools emphasize the importance of hospital-based early clinical exposure during pre-clerkship years. The COVID-19 pandemic is causing major disturbances to classroom and hospital training environments, placing these foundations for a successful medical education at great risk [4]. Social distancing, as recommended by the Centers for Disease Control and Prevention (CDC), remains a powerful measure to retard the pandemic’s growth [5]. Therefore, one swift change many medical schools adopted was cancellation of in-person classes and moving to pre-recorded or live-streamed lectures [6]. The loss of a group experience and in-person feedback offered in a classroom setting may eventually be unfavorable to student learning, especially for those who thrive in an in-person learning environment [7]. In order to remedy this learning gap, medical schools have also turned to online platforms like Zoom, which allow interactive group discussions [8]. While the movement to online curricula does accommodate social distancing guidelines and may satisfy some of the requirements for undergraduate medical education [9], its outcomes and effectiveness are unclear and may potentially be suboptimal in graduate medical education [10], where a greater degree of hands-on experience is crucial to learning many patient care skills.
The COVID-19 pandemic continues to have a negative impact on student learning during their clerkship years. Many schools have cancelled clinical clerkships in an effort to limit personal interaction in the hospital, conserve personal protective equipment, and reduce the risk of exposure for their students [11]. Other factors that limit student clinical participation in the clinical environment include the shortages of COVID-19 testing [12], cancelation of elective surgical procedures [13], and increased use of telehealth [14]. This presents a challenge to providing students with authentic patient experiences [15]. Educators are increasingly moving clinical experiences to an online format, deferring clinical time to a later date, or incorporating virtual case studies in education [16]. Current options remain limited and are forcing several revolutionary changes to the traditional tools of medical education [17], calling for innovative novel strategies to address the issue [18]. Ongoing re-evaluation of the pandemic’s impact on clinical education is necessary so medical schools can decide on effective and sustainable policies [19].
Graduate medical education has also seen many challenges and innovations as a result of the pandemic [20]. Residents and fellows are already seeing a change in patient relationship as the pandemic evolves, with reliance on technology to fill in the gaps in traditional bedside teaching [21]. Fellowship training overall may have a greater requirement for procedural competencies which are difficult to accommodate because of the COVID-19 pandemic. The exponential numbers of COVID-19 cases in certain states has called for deployment of fellow trainees, especially in cardiology [22], to care for such patients, as allowed by the Accreditation Commission on Graduate Medical Education (ACGME), which understandably takes away from the time for fellowship training. Several major medical and surgical societies, including the American College of Cardiology (ACC), recommended limiting elective surgeries and procedures, including cardiac procedures, and curtailing trainee role in urgent procedures involving COVID-19 confirmed or suspect patients in order to reduce infection exposure [23]. Moreover, the role of interventional cardiac procedures in the care of COVID-19 patients has also diminished with greater reliance on non-interventional treatments [24]. Such limitations have placed tremendous strain on fellowships, especially in interventional cardiology, requiring tailored training strategies to provide adequate procedural competencies [25]. The American Society of Echocardiography (ASE) provided a guidance statement for the provision of echocardiography services during the COVID-19 pandemic, which would be expected to limit the number of echocardiography procedures and likely impact fellowship training in cardiology as well [26]. The extent to which all these unprecedented constraints will impact the quality of education in cardiology and other fellowship training remains unknown and would need careful evaluation and mitigation [27].
The Future
The COVID-19 pandemic has unequivocally resulted in major transformations to the undergraduate and graduate medical education, calling for timely innovations and modernization. While all aspects of education have been affected by the pandemic, the impact has been greatest on advanced training in cardiology and procedural competencies in the US and other countries [28]. This has created tremendous angst amongst training programs as nontraditional and less-proven methods of education had to be adopted. Reliance on less sophisticated tool for diagnosis may provide an opportunity to revive the role of the stethoscope in medical training in general and cardiology training in particular [29]. However, the cardiology field has come very far in providing high tech diagnostic and therapeutic procedures proven to impact morbidity and mortality, which require rigorous training according to strict guidelines. The expectation is that future generations of cardiologists will not only be competent in such procedures, but also be able to provide further innovations which will continue to improve patient outcomes. Development of procedural competencies may require increased reliance on robust simulation tools to prepare trainees and reduce their encounter time with real patients [30]. Humanity has suffered unfathomable distress from the pandemic at multiple levels, most importantly education; the response has been substantial concerted crisis-driven innovations which will hopefully positively guide future generations.
References:
- Nicola M, Alsafi Z, Sohrabi C, et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int J Surg. 2020;78:185-193.
- Chiodini J. Online learning in the time of COVID-19. Travel Med Infect Dis. 2020;34:101669.
- Akkermans J, Richardson J, Kraimer M. The Covid-19 crisis as a career shock: Implications for careers and vocational behavior. J Vocat Behav. 2020;119:103434.
- Rose S. Medical Student Education in the Time of COVID-19. JAMA. 2020;323(21):2131–2132.
- Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures In The United States Reduced The COVID-19 Growth Rate. Health Aff (Millwood). 2020;39(7):1237-1246.
- Ferrel MN, Ryan JJ. The Impact of COVID-19 on Medical Education. Cureus. 2020;12(3):e7492. Published 2020 Mar 31.
- Seymour-Walsh AE, Bell A, Weber A, Smith T. Adapting to a new reality: COVID-19 coronavirus and online education in the health professions. Rural Remote Health. 2020;20(2):6000.
- O'Doherty D, Dromey M, Lougheed J, Hannigan A, Last J, McGrath D. Barriers and solutions to online learning in medical education - an integrative review. BMC Med Educ. 2018;18(1):130. Published 2018 Jun 7.
- Sandhu P, de Wolf M. The impact of COVID-19 on the undergraduate medical curriculum. Med Educ Online. 2020;25(1):1764740.
- Almarzooq ZI, Lopes M, Kochar A. Virtual Learning During the COVID-19 Pandemic: A Disruptive Technology in Graduate Medical Education. J Am Coll Cardiol. 2020;75(20):2635-2638.
- O'Sullivan ED. PPE guidance for covid-19: be honest about resource shortages. BMJ. 2020;369:m1507.
- Beetz C, Skrahina V, Förster TM, et al. Rapid Large-Scale COVID-19 Testing During Shortages. Diagnostics (Basel). 2020;10(7):E464. Published 2020 Jul 8.
- COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans [published online ahead of print, 2020 May 12]. Br J Surg. 2020;10.1002/bjs.11746.
- Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957-962.
- Hammond D, Louca C, Leeves L, Rampes S. Undergraduate medical education and Covid-19: engaged but abstract. Med Educ Online. 2020;25(1):1781379.
- Remtulla R. The Present and Future Applications of Technology in Adapting Medical Education Amidst the COVID-19 Pandemic. JMIR Med Educ. 2020;6(2):e20190. Published 2020 Jul 17.
- Torda A. How COVID-19 has pushed us into a medical education revolution [published online ahead of print, 2020 Jul 14]. Intern Med J. 2020;10.1111/imj.14882.
- Watson A, McKinnon T, Prior SD, Richards L, Green CA. COVID-19: time for a bold new strategy for medical education. Med Educ Online. 2020;25(1):1764741
- Chen CH, Mullen AJ. COVID-19 Can Catalyze the Modernization of Medical Education. JMIR Med Educ. 2020;6(1):e19725. Published 2020 Jun 12.
- Dedeilia A, Sotiropoulos MG, Hanrahan JG, Janga D, Dedeilias P, Sideris M. Medical and Surgical Education Challenges and Innovations in the COVID-19 Era: A Systematic Review. In Vivo. 2020;34(3 Suppl):1603-1611.
- Chick RC, Clifton GT, Peace KM, et al. Using Technology to Maintain the Education of Residents During the COVID-19 Pandemic. J Surg Educ. 2020;77(4):729-732.
- Gallagher MJ, Bloomingdale R, Berman AD, Williamson BD, Dixon SR, Safian RD. Strategic Deployment of Cardiology Fellows in Training Using the Accreditation Council for Graduate Medical Education Coronavirus Disease 2019 Framework. J Am Heart Assoc. 2020;9(14):e017443.
- Nguyen L, Sachdev S, Tahir H, et al. COronaVIrus Disease 2019 (COVID-19) & The Cardiology Consultant. Cardiofel Newslet 2020 April; 3(4):15-20.
- Sachdev S, Tahir H, Nguyen L, et al. COVID-19 and Interventional Cardiology: To Cath or Not to Cath! That May Not Be The Only Question!. Cardiofel Newslet 2020. May; 3(5):21-25.
- Gupta T, Nazif TM, Vahl TP, et al. Impact of the COVID-19 pandemic on interventional cardiology fellowship training in the New York metropolitan area: A perspective from the United States epicenter [published online ahead of print, 2020 May 16]. Catheter Cardiovasc Interv. 2020;10.1002/ccd.28977.
- Bardia N, Nwokeocha N, Tahir H, et al. Echocardiography in the COVID 19 Pandemic – Whom, Where & How? Cardiofel Newslet 2020. March; 3(3):13 – 14.
- Potts JR 3rd. Residency and Fellowship Program Accreditation: Effects of the Novel Coronavirus (COVID-19) Pandemic. J Am Coll Surg. 2020;230(6):1094-1097.
- Lim Y, Chook S, Low TT, Yeo WT, Tay E. Cardiology Training in Singapore During the COVID-19 Pandemic. Acad Med.2020;10.1097/ACM.0000000000003570
- Vasudevan RS, Horiuchi Y, Torriani FJ, et al. Persistent Value of the Stethoscope in the Age of COVID-19, 2020 Jun 19]. Am J Med. 2020;S0002-9343(20)30508-8.
- Westerdahl DE. The Necessity of High-Fidelity Simulation in Cardiology Training Programs. J Am Coll Cardiol. 2016;67(11):1375-1378.
Authors:
Saad Awan, B.S.
Medical Student
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL