July 2022 Issue
ISSN 2689-291X
ISSN 2689-291X
Bacterial Pericarditis:
Loculation Requiring Pericardiectomy!
Description
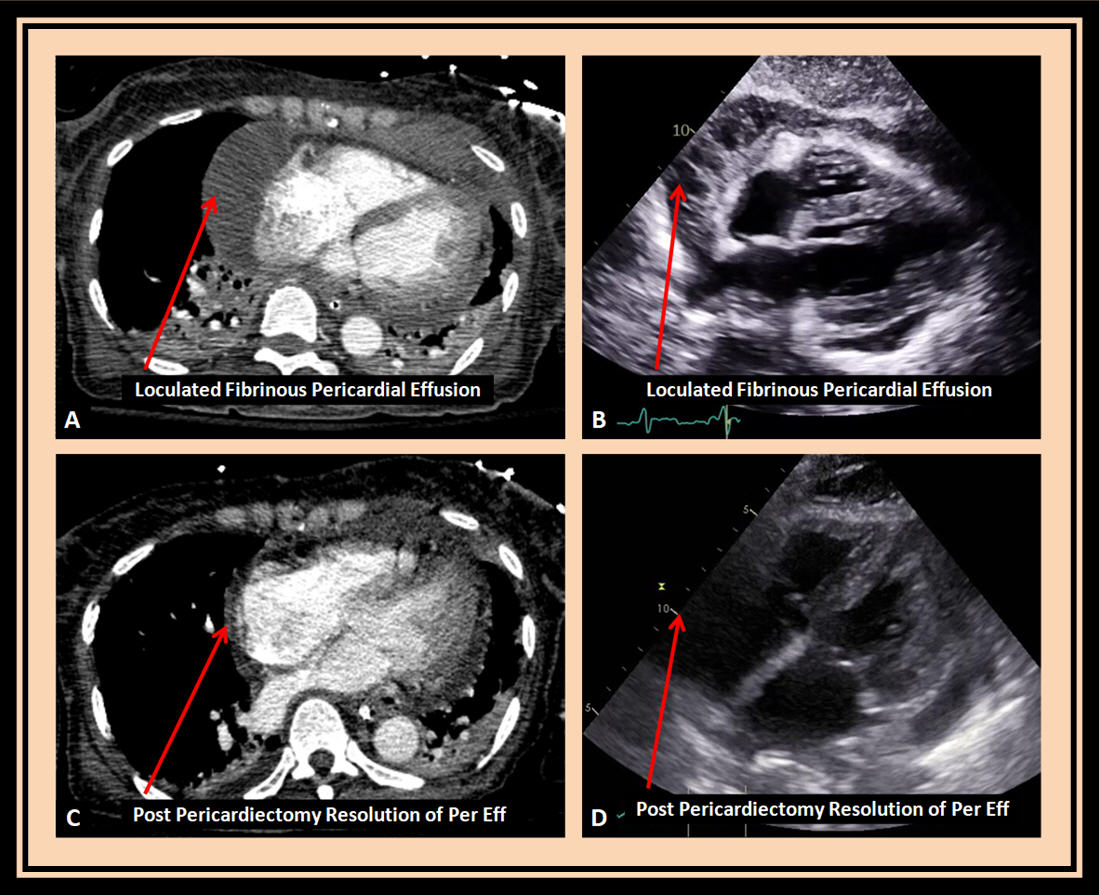
The above coronal computed tomography (CT) image (A) and subcostal transthoracic echocardiography (TTE) image (B) reveal a highly fibrinous pericardial effusion, recurrent following initial pericardial window, with multiple loculations, especially along the right atrial and right ventricular borders; initial pericardial fluid cultures grew Streptococcus pneumoniae.
Further percutaneous drainage was deemed not feasible due to excessive adhesions. Persistent fever and positive blood cultures prompted successful widespread pericardiectomy of the majority of the anterior and part of the posterior pericardium with resultant resolution of the loculation on CT (C) and TTE (D) corresponding images, resulting in clinical improvement.
Discussion
Bacterial pericarditis is a serious infection involving the pericardial fluid with high morbidity, and mortality of up to 85% if untreated and nearly 40% with treatment [1]. Although in the majority of cases infectious pericarditis is secondary to procedures or manipulation close to the pericardium, rare cases of primary bacterial pericarditis, without any demonstrable cause, have been reported [2].
Several pathogens have been reported to cause bacterial pericarditis, most commonly Staphylococcus and Streptococcus species. A case of bacterial pericarditis due to Staphylococcus aureus was reported leading to cardiogenic shock, and was successfully treated with pericardial drainage and antibiotics [3]. Another case of primary bacterial pericarditis due to Streptococcus pneumoniae was reported which also responded to drainage and antibiotics [4].
Bacterial pericarditis can lead to rapid pericardial fluid accumulation leading to cardiac tamponade and empyema which may be fatal if not treated promptly [5]. Constrictive pericarditis necessitating Pericardiectomy despite initial fluid drainage and antibiotics is also a reported complication of bacterial pericarditis [6].
Several predisposing conditions and compromised immune status have been linked to infectious pericarditis. Bacterial pericarditis due to Streptococcus hominis was reported in a patient 18 days following COVID-19 infection, and treated successfully with drainage and antibiotics [7].
Iatrogenic bacterial pericarditis can directly or indirectly be related to intra-abdominal procedure. Polymicrobial pericarditis has been reported due to penetration of the pericardium by catheter tip in a laparoscopic adjustable gastric band, leading to tamponade [8]. Another case of bacterial pericarditis due to biliary stent migration and penetration of the pericardium has been reported [9].
A retrospective review of 33 cases of purulent pericarditis concluded that the condition does not cause classic findings of pericarditis and is often diagnosed late with tamponade or at autopsy [10]. It is imperative to maintain a high index of suspicious of bacterial pericarditis in patients with infection and any hemodynamic alterations so as prompt life-saving treatment can be implemented.
References
Authors:
Douglas Williams, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, A
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The above coronal computed tomography (CT) image (A) and subcostal transthoracic echocardiography (TTE) image (B) reveal a highly fibrinous pericardial effusion, recurrent following initial pericardial window, with multiple loculations, especially along the right atrial and right ventricular borders; initial pericardial fluid cultures grew Streptococcus pneumoniae.
Further percutaneous drainage was deemed not feasible due to excessive adhesions. Persistent fever and positive blood cultures prompted successful widespread pericardiectomy of the majority of the anterior and part of the posterior pericardium with resultant resolution of the loculation on CT (C) and TTE (D) corresponding images, resulting in clinical improvement.
Discussion
Bacterial pericarditis is a serious infection involving the pericardial fluid with high morbidity, and mortality of up to 85% if untreated and nearly 40% with treatment [1]. Although in the majority of cases infectious pericarditis is secondary to procedures or manipulation close to the pericardium, rare cases of primary bacterial pericarditis, without any demonstrable cause, have been reported [2].
Several pathogens have been reported to cause bacterial pericarditis, most commonly Staphylococcus and Streptococcus species. A case of bacterial pericarditis due to Staphylococcus aureus was reported leading to cardiogenic shock, and was successfully treated with pericardial drainage and antibiotics [3]. Another case of primary bacterial pericarditis due to Streptococcus pneumoniae was reported which also responded to drainage and antibiotics [4].
Bacterial pericarditis can lead to rapid pericardial fluid accumulation leading to cardiac tamponade and empyema which may be fatal if not treated promptly [5]. Constrictive pericarditis necessitating Pericardiectomy despite initial fluid drainage and antibiotics is also a reported complication of bacterial pericarditis [6].
Several predisposing conditions and compromised immune status have been linked to infectious pericarditis. Bacterial pericarditis due to Streptococcus hominis was reported in a patient 18 days following COVID-19 infection, and treated successfully with drainage and antibiotics [7].
Iatrogenic bacterial pericarditis can directly or indirectly be related to intra-abdominal procedure. Polymicrobial pericarditis has been reported due to penetration of the pericardium by catheter tip in a laparoscopic adjustable gastric band, leading to tamponade [8]. Another case of bacterial pericarditis due to biliary stent migration and penetration of the pericardium has been reported [9].
A retrospective review of 33 cases of purulent pericarditis concluded that the condition does not cause classic findings of pericarditis and is often diagnosed late with tamponade or at autopsy [10]. It is imperative to maintain a high index of suspicious of bacterial pericarditis in patients with infection and any hemodynamic alterations so as prompt life-saving treatment can be implemented.
References
- Pankuweit S, Ristić AD, Seferović PM, Maisch B. Bacterial pericarditis: diagnosis and management. Am J Cardiovasc Drugs. 2005;5(2):103-12.
- Keersmaekers T, Elshot SR, Sergeant PT. Primary bacterial pericarditis. Acta Cardiol. 2002 Oct;57(5):387-9.
- Kaye A, Peters GA, Joseph JW, Wong ML. Purulent bacterial pericarditis from Staphylococcus aureus. Clin Case Rep. 2019 May 28;7(7):1331-1334.
- Khan MS, Khan Z, Banglore BS, Alkhoury G, Murphy L, Georgescu C. Primary purulent bacterial pericarditis due to Streptococcus intermedius in an immunocompetent adult: a case report. J Med Case Rep. 2018 Feb 5;12(1):27.
- Kondapi D, Markabawi D, Chu A, Gambhir HS. Staphylococcal Pericarditis Causing Pericardial Tamponade and Concurrent Empyema. Case Rep Infect Dis. 2019 Jul 18;2019:3701576.
- Koster N, Narmi A, Anand K. Bacterial pericarditis. Am J Med. 2009 May;122(5):e1-2.
- Sagristà-Sauleda J, Barrabés JA, Permanyer-Miralda G, Soler-Soler J. Purulent pericarditis: review of a 20-year experience in a general hospital. J Am Coll Cardiol. 1993 Nov 15;22(6):1661-5.
- Chao HY, Li CH, Chen SY. Bacterial Pericarditis Caused by Penetration of a Migrated Biliary Stent from the Lateral Segment of the Liver: A Case Report. Medicina (Kaunas). 2022 Jan 15;58(1):132.
- Lee PH, Tan HL, Chia YW, Ling LM. A case of acute bacterial pericarditis in a COVID-19 patient. Singapore Med J. 2022 Aug;63(8):484-486.
- de Jong Y, van Loenhout RB, Swank DJ, Jansen CL, Sorgdrager BJ. Polymicrobial bacterial pericarditis and cardiac tamponade caused by pericardial penetration of an adjustable gastric band. BMJ Case Rep. 2018 Feb 16;2018:bcr2017221589.
Authors:
Douglas Williams, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, A
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL