June 2020 Issue
ISSN 2689-291X
ISSN 2689-291X
Echocardiography in the COVID 19 Pandemic –
Whom, Where & How?
Introduction:
The COVID 19 pandemic has already affected about 2.25 million individuals and claimed the lives of approximately 120,000 individuals in the United States alone [1], placing previously unimaginable strain on the health care system [2]. The pandemic, which has a high affinity for the cardiovascular system, has also introduced novel challenges for the cardiology consultant in general [3], and for the provision of diagnostic and therapeutic cardiovascular modalities such as interventional cardiology services [4]. The general theme has been to provide high quality care and testing which is urgently needed to save lives in the most efficient and safe manner while protecting the healthcare personnel and equipment from exposure to infection [5]. This meant that many indicated but not urgent procedures must be postponed until the risk of infection can be minimized [6].
Statement:
The newly published ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak [7] provides valuable guidance on the provision of echocardiography services during the COVID pandemic in terms of who, where and how to image. The statement recognizes the importance of dedication to patient care and the fact that healthcare providers must care for themselves, their loved ones and prevent the spread of disease to their patients, by reducing their own risk and using proper personal protective equipment (PPE).
With regards to whom to image, this involves careful review of the indications and appropriate use criteria, employing one of two strategies: 1. rescheduling “elective” studies, while performing all others, 2. performing “nonelective” (urgent or emergent) studies while postponing all others. Therefore, a study should be performed if the information obtained would provide immediate clinical benefit and deferring the study may result in clinical harm. If the COVID status is confirmed positive or unknown, then proper PPE must be applied. Specialized procedures such as transesophageal echocardiography and stress echocardiography may present higher risk of droplet infection due to patient’s gag, cough and deep breathing, and alternative testing should be sought if at all possible.
With regards to where to image, bedside echocardiography should be employed when feasible to minimize spread of infection since many of these patients are in isolation room, despite the disadvantage of not using specialized echocardiography beds. Screening of outpatients according to established hospital protocols may also help mitigate the risk of exposure of personnel in the outpatient setting.
With regards to how to image, this involves employing different protocols, the use of PPE, the role of learners in addition to other considerations. Ultrasound-assisted physical examination (UAPE) and point-of-care cardiac ultrasound (POCUS), performed bedside by the provider caring for COVID or suspect patients to screen for cardiac disease are safer alternatives to full transthoracic echocardiography. Studies should be planned ahead of time with regards to obtaining the most informative views in the shortest time possible to reduce exposure; this requires experienced sonographers and exclusion of learners. Saving images from such studies or having remote capability for review by a cardiologist can provide prompt interpretation and obviate the need for further studies, thereby reducing exposure. When studies are being performed, the proper use of PPE with regards to hand sanitization, droplet and airborne precautions, and shoe covers should be strictly enforced by personnel, together with equipment protection using plastic covers and later application of proper sterilization techniques. Learners’ role should be limited given to longer time they need to image, and training requirements can be supplemented with available online education. Other considerations involve limiting the role of vulnerable personnel who are older than 60 years of age, have chronic conditions, are immunocompromised, or are pregnant. Limiting congregation of various physicians in echo reading rooms should also be enforced by allowing for online access of image which can be reviewed with the reading physician remotely and rapid availability of echocardiography final reports.
Conclusion:
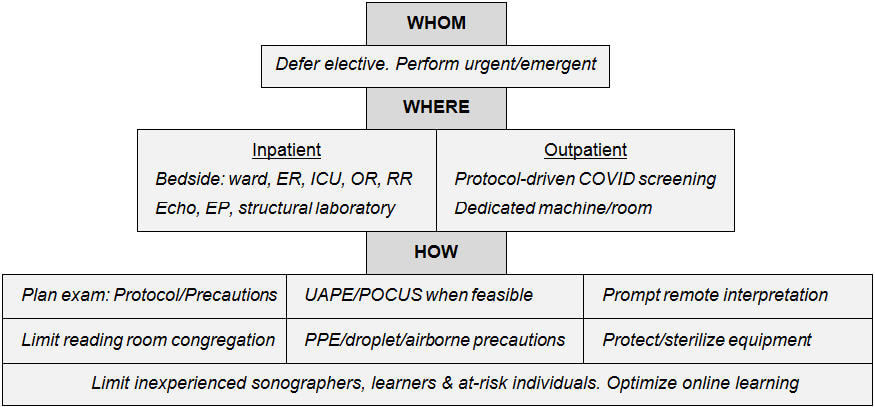
Applying the whom, where and how to image algorithm suggested by the ASE new statement provides an important framework for the provision of echocardiographic studies during the COVID 19 pandemic in the safest manner that protects patients and personnel (table 1). Implementation of such framework is expected to minimize the spread of infection and provide a safer environment for all involved personnel while providing targeted and meaningful echocardiographic examinations.
References
Table 1. Summary of the “whom, where and how” approach to provision of echocardiographic studies during the COVD-19 pandemic to COVID/suspect patients based on ASE statement [7].
The COVID 19 pandemic has already affected about 2.25 million individuals and claimed the lives of approximately 120,000 individuals in the United States alone [1], placing previously unimaginable strain on the health care system [2]. The pandemic, which has a high affinity for the cardiovascular system, has also introduced novel challenges for the cardiology consultant in general [3], and for the provision of diagnostic and therapeutic cardiovascular modalities such as interventional cardiology services [4]. The general theme has been to provide high quality care and testing which is urgently needed to save lives in the most efficient and safe manner while protecting the healthcare personnel and equipment from exposure to infection [5]. This meant that many indicated but not urgent procedures must be postponed until the risk of infection can be minimized [6].
Statement:
The newly published ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak [7] provides valuable guidance on the provision of echocardiography services during the COVID pandemic in terms of who, where and how to image. The statement recognizes the importance of dedication to patient care and the fact that healthcare providers must care for themselves, their loved ones and prevent the spread of disease to their patients, by reducing their own risk and using proper personal protective equipment (PPE).
With regards to whom to image, this involves careful review of the indications and appropriate use criteria, employing one of two strategies: 1. rescheduling “elective” studies, while performing all others, 2. performing “nonelective” (urgent or emergent) studies while postponing all others. Therefore, a study should be performed if the information obtained would provide immediate clinical benefit and deferring the study may result in clinical harm. If the COVID status is confirmed positive or unknown, then proper PPE must be applied. Specialized procedures such as transesophageal echocardiography and stress echocardiography may present higher risk of droplet infection due to patient’s gag, cough and deep breathing, and alternative testing should be sought if at all possible.
With regards to where to image, bedside echocardiography should be employed when feasible to minimize spread of infection since many of these patients are in isolation room, despite the disadvantage of not using specialized echocardiography beds. Screening of outpatients according to established hospital protocols may also help mitigate the risk of exposure of personnel in the outpatient setting.
With regards to how to image, this involves employing different protocols, the use of PPE, the role of learners in addition to other considerations. Ultrasound-assisted physical examination (UAPE) and point-of-care cardiac ultrasound (POCUS), performed bedside by the provider caring for COVID or suspect patients to screen for cardiac disease are safer alternatives to full transthoracic echocardiography. Studies should be planned ahead of time with regards to obtaining the most informative views in the shortest time possible to reduce exposure; this requires experienced sonographers and exclusion of learners. Saving images from such studies or having remote capability for review by a cardiologist can provide prompt interpretation and obviate the need for further studies, thereby reducing exposure. When studies are being performed, the proper use of PPE with regards to hand sanitization, droplet and airborne precautions, and shoe covers should be strictly enforced by personnel, together with equipment protection using plastic covers and later application of proper sterilization techniques. Learners’ role should be limited given to longer time they need to image, and training requirements can be supplemented with available online education. Other considerations involve limiting the role of vulnerable personnel who are older than 60 years of age, have chronic conditions, are immunocompromised, or are pregnant. Limiting congregation of various physicians in echo reading rooms should also be enforced by allowing for online access of image which can be reviewed with the reading physician remotely and rapid availability of echocardiography final reports.
Conclusion:
Applying the whom, where and how to image algorithm suggested by the ASE new statement provides an important framework for the provision of echocardiographic studies during the COVID 19 pandemic in the safest manner that protects patients and personnel (table 1). Implementation of such framework is expected to minimize the spread of infection and provide a safer environment for all involved personnel while providing targeted and meaningful echocardiographic examinations.
References
- CDC, Coronavirus Disease 2019 (COVID-19), Cases, Data & Surveillance, Cases & Deaths in the US. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html.
- Ji Y, Ma Z, Peppelenbosch MP, Pan Q. Potential association between COVID-19 mortality and health-care resource availability. Lancet Glob Health. 2020;8(4):e480.
- Landai N, Sachdev S, Tahir H, et al. COronaVIrus Disease 2019 (COVID-19) & The Cardiology Consultant. Cardiofel Newslet 2020 April; 3(4):15-20.
- Sachdev S, Tahir H, Nguyen L, et al. COVID-19 and Interventional Cardiology: To Cath or Not to Cath! That May Not Be The Only Question! Cardiofel Newslet 2020. May; 3(5):21-25.
- Koh D. Occupational risks for COVID-19 infection. Occup Med (Lond). 2020;70(1):3-5.
- CMS Releases Recommendations on Adult Elective Surgeries, Non-Essential Medical, Surgical, and Dental Procedures During COVID-19 Response. https://www.cms.gov/newsroom/press-releases/cms-releases-recommendations-adult-elective-surgeries-non-essential-medical-surgical-and-dental.
- Kirkpatrick JN, Mitchell C, Taub C, et el. ASE Statement on Protection of Patients and Echocardiography Service Providers During the 2019 Novel Coronavirus Outbreak: Endorsed by the American College of Cardiology. J Am Coll Cardiol. 2020 Jun 23;75(24):3078-3084.
Table 1. Summary of the “whom, where and how” approach to provision of echocardiographic studies during the COVD-19 pandemic to COVID/suspect patients based on ASE statement [7].
Abbreviations: ER: emergency room; ICU: intensive care unit; OR: operating room; RR: recovery room; Echo: echocardiography; EP: electrophysiology; UAPE: ultrasound-assisted physical examination; POCUS: point of care ultrasound; PPE: personal protective equipment.
Authors:
Nikky Bardia, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nneka Nwokeocha, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Hassan Tahir, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Authors:
Nikky Bardia, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nneka Nwokeocha, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Hassan Tahir, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Landai Nguyen, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL