May 2021 Issue
ISSN 2689-291X
ISSN 2689-291X
Yamaguchi Cardiomyopathy..
The Ace-Of-Spades!
Description
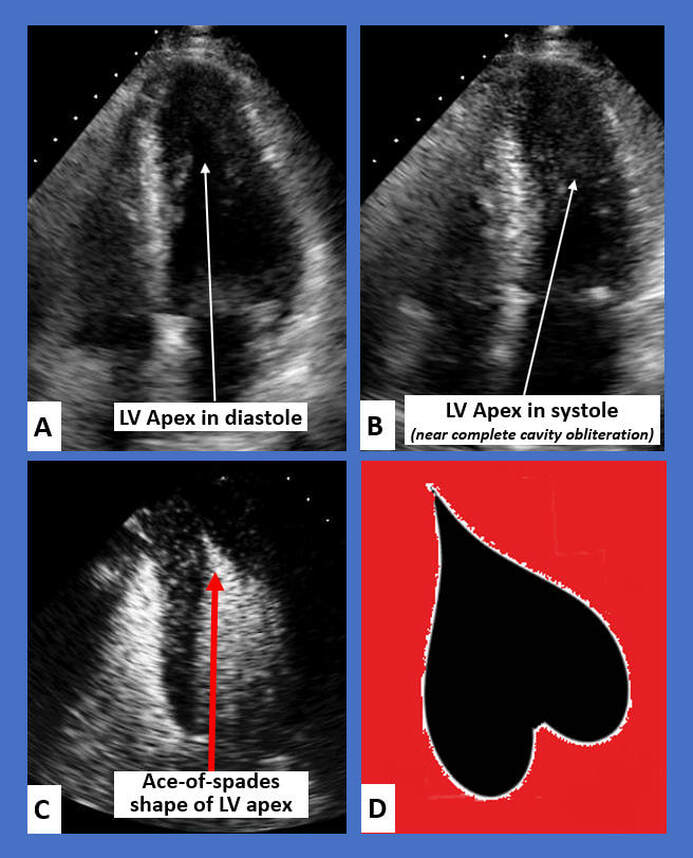
The figure above shows 2-D echocardiographic images in apical hypertrophic cardiomyopathy, also referred to as Yamaguchi syndrome. Figure A shows the thickening of the mid to apical wall segments of the left ventricle (LV) in diastole, while figure B shows the near complete obliteration of the LV apical cavity in systole due to the hypertrophy. Figure C demonstrates to characteristic Ace-of-spades appearance of the LV using Optison contrast, as depicted in the cartoon in figure D.
Discussion
Yamaguchi cardiomyopathy is a non-obstructive hypertrophic cardiomyopathy characterized by apical hypertrophy. There is hypertrophy of the myocardium in the apex of left ventricle while the septum is relatively unremarkable [1]. This cardiomyopathy is found predominantly in the Japanese population [2]. The female to male prevalence is approximately 2:1 [3]. There have been several genes associated involving sarcomere proteins. It usually transmitted in an autosomal dominant manner with incomplete penetrance similar to other forms of cardiomyopathy [4].
There is wide spectrum of clinical presentations in apical hypertrophic cardiomyopathy including angina, palpitations, and presyncope/syncope. Due to a lack of septal involvement, there is no left ventricular outflow tract obstruction and therefore no outflow tract murmur is expected on exam [5].
Electrocardiography shows left ventricular hypertrophy in the absence of hypertension or aortic stenosis and T-wave inversion of >10 mm in the precordial leads [6]. Echocardiography is required for diagnosis. It shows a classic “Ace-of-spades” pattern at end of diastole [7]. In certain patients with difficulty imaging of the cardiac apex, cardiac MRI may be warranted. Cardiac MRI is more sensitive in detecting apical aneurysms and the amount of apical late gadolinium enhancement describes the severity of the hypertrophy, yet it is not required for diagnosis [8]. Often advanced multimodality imaging will need to be employed for the proper diagnosis and prognosis of this cardiomyopathy [9, 10].
There are three subtypes of apical hypertrophic cardiomyopathy [11], 1) pure, isolated apical hypertrophy, 2) mixed, apical hypertrophy greater than septal hypertrophy, and 3) relative, slight apical hypertrophy. Relative subtype is thought to be early form of the phenotype. Patients with mixed subtype, earlier onset of presentation, apical akinesis, end systolic ventricular obliteration, and paradoxical diastolic flow jet have higher rates of morbidity. Patients develop atrial and ventricular arrhythmias.
Management strategies are aimed at preventing cardiac remodeling, minimizing symptoms, and treatment of arrhythmias [12]. ACE-inhibitors are shown to reduce afterload and adverse cardiac remodeling. Both beta-blockers and calcium channel blockers have been used for symptom reduction. Patients with severe diastolic dysfunction leading to atrial arrhythmias may require anticoagulation for stroke prevention. Patients with high risk of mortality will benefit from dual chamber pacemaker [13].
References:
Authors:
Akhil Padarti, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The figure above shows 2-D echocardiographic images in apical hypertrophic cardiomyopathy, also referred to as Yamaguchi syndrome. Figure A shows the thickening of the mid to apical wall segments of the left ventricle (LV) in diastole, while figure B shows the near complete obliteration of the LV apical cavity in systole due to the hypertrophy. Figure C demonstrates to characteristic Ace-of-spades appearance of the LV using Optison contrast, as depicted in the cartoon in figure D.
Discussion
Yamaguchi cardiomyopathy is a non-obstructive hypertrophic cardiomyopathy characterized by apical hypertrophy. There is hypertrophy of the myocardium in the apex of left ventricle while the septum is relatively unremarkable [1]. This cardiomyopathy is found predominantly in the Japanese population [2]. The female to male prevalence is approximately 2:1 [3]. There have been several genes associated involving sarcomere proteins. It usually transmitted in an autosomal dominant manner with incomplete penetrance similar to other forms of cardiomyopathy [4].
There is wide spectrum of clinical presentations in apical hypertrophic cardiomyopathy including angina, palpitations, and presyncope/syncope. Due to a lack of septal involvement, there is no left ventricular outflow tract obstruction and therefore no outflow tract murmur is expected on exam [5].
Electrocardiography shows left ventricular hypertrophy in the absence of hypertension or aortic stenosis and T-wave inversion of >10 mm in the precordial leads [6]. Echocardiography is required for diagnosis. It shows a classic “Ace-of-spades” pattern at end of diastole [7]. In certain patients with difficulty imaging of the cardiac apex, cardiac MRI may be warranted. Cardiac MRI is more sensitive in detecting apical aneurysms and the amount of apical late gadolinium enhancement describes the severity of the hypertrophy, yet it is not required for diagnosis [8]. Often advanced multimodality imaging will need to be employed for the proper diagnosis and prognosis of this cardiomyopathy [9, 10].
There are three subtypes of apical hypertrophic cardiomyopathy [11], 1) pure, isolated apical hypertrophy, 2) mixed, apical hypertrophy greater than septal hypertrophy, and 3) relative, slight apical hypertrophy. Relative subtype is thought to be early form of the phenotype. Patients with mixed subtype, earlier onset of presentation, apical akinesis, end systolic ventricular obliteration, and paradoxical diastolic flow jet have higher rates of morbidity. Patients develop atrial and ventricular arrhythmias.
Management strategies are aimed at preventing cardiac remodeling, minimizing symptoms, and treatment of arrhythmias [12]. ACE-inhibitors are shown to reduce afterload and adverse cardiac remodeling. Both beta-blockers and calcium channel blockers have been used for symptom reduction. Patients with severe diastolic dysfunction leading to atrial arrhythmias may require anticoagulation for stroke prevention. Patients with high risk of mortality will benefit from dual chamber pacemaker [13].
References:
- Hughes RK, Knott KD, Malcolmson J, Augusto JB, Mohiddin SA, Kellman P, Moon JC, Captur G. Apical Hypertrophic Cardiomyopathy: The Variant Less Known. J Am Heart Assoc. 2020 Mar 3;9(5):e015294.
- Kitaoka H, Doi Y, Casey SA, Hitomi N, Furuno T, Maron BJ. Comparison of prevalence of apical hypertrophic cardiomyopathy in Japan and the United States. Am J Cardiol. 2003 Nov 15;92(10):1183-6.
- Kubo T, Kitaoka H, Okawa M, Hirota T, Hayato K, Yamasaki N, Matsumura Y, Yabe T, Doi YL. Gender-specific differences in the clinical features of hypertrophic cardiomyopathy in a community-based Japanese population: results from Kochi RYOMA study. J Cardiol. 2010 Nov;56(3):314-9.
- Towe EC, Bos JM, Ommen SR, Gersh BJ, Ackerman MJ. Genotype-Phenotype Correlations in Apical Variant Hypertrophic Cardiomyopathy. Congenit Heart Dis. 2015 May-Jun;10(3):E139-45.
- Paluszkiewicz J, Krasinska B, Milting H, Gummert J, Pyda M. Apical hypertrophic cardiomyopathy: diagnosis, medical and surgical treatment. Kardiochir Torakochirurgia Pol. 2018 Dec;15(4):246-253.
- Madias JE. Electrocardiogram in apical hypertrophic cardiomyopathy with a speculation as to the mechanism of its features. Neth Heart J. 2013 Jun;21(6):268-71.
- Diaconu CC, Dumitru N, Fruntelata AG, Lacau S, Bartos D. Apical Hypertrophic Cardiomyopathy: The Ace-of-Spades as the Disease Card. Acta Cardiol Sin. 2015 Jan;31(1):83-6.
- Ibrahim T, Schwaiger M. Diagnosis of apical hypertrophic cardiomyopathy using magnetic resonance imaging. Heart. 2000 Jan;83(1):E1.
- Hughes RK, Knott KD, Malcolmson J, Augusto JB, Kellman P, Moon JC, Captur G. Advanced Imaging Insights in Apical Hypertrophic Cardiomyopathy. JACC Cardiovasc Imaging. 2020 Feb;13(2 Pt 2):624-630.
- Huang G, Fadl SA, Sukhotski S, Matesan M. Apical variant hypertrophic cardiomyopathy "multimodality imaging evaluation". Int J Cardiovasc Imaging. 2020 Mar;36(3):553-561.
- Sherrid MV, Massera D. Risk Stratification and Hypertrophic Cardiomyopathy Subtypes. J Am Coll Cardiol. 2019 Nov 12;74(19):2346-2349.
- Jan MF, Todaro MC, Oreto L, Tajik AJ. Apical hypertrophic cardiomyopathy: Present status. Int J Cardiol. 2016 Nov 1;222:745-759.
- Wever-Pinzon O, Romero J, Cordova JP. Dual chamber pacing relieves obstruction in Japanese-variant hypertrophic cardiomyopathy. Am J Ther. 2013 Sep-Oct;20(5):588-90.
Authors:
Akhil Padarti, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL