November 2022 Issue
ISSN 2689-291X
ISSN 2689-291X
Bladder Pacemaker:
Electrocardiographic Interference!
Description
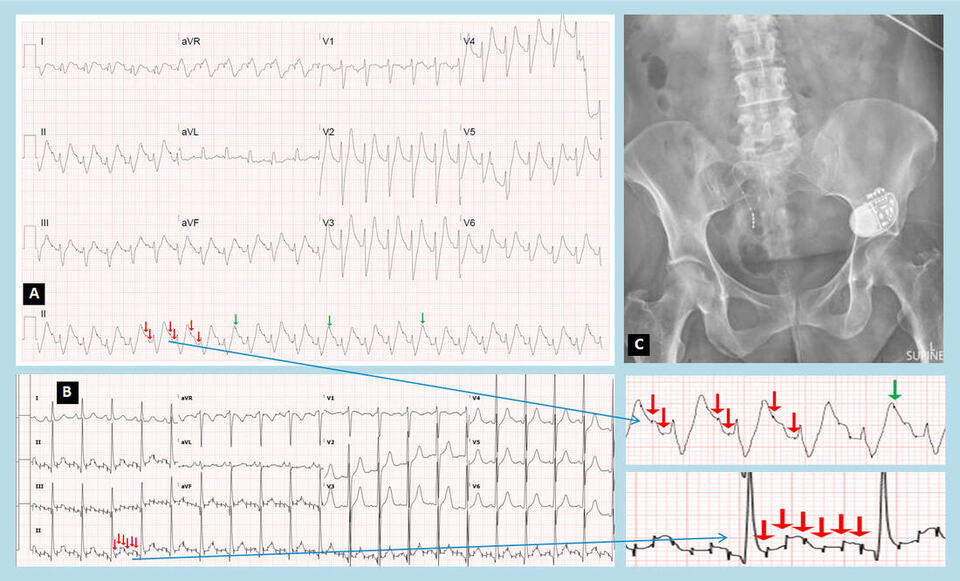
The above electrocardiogram (EKG) in Figure A reveals pacemaker spikes preceding a wide QRS complex rhythm initially suggestive of dual chamber (AV sequential) pacing. Closer scrutiny (insert) reveals additional pacemaker spikes on the T waves which are inappropriate and do not support a pacing role for the detected spikes. Review of a prior EKG in Figure B revealed very fast pacing spikes with a cycle length of approximately 77 ms, and a rate of about 780/minute, thought to be AC interference (insert). The Chest X ray did not reveal evidence of any cardiac pacemaker. A Kidney, Ureter and Bladder (KUB) X ray, however, revealed a bladder pacemaker historically placed for atonic bladder as the cause for this interference artifact, likely set at 13 Hz, as seen in Figure C. The EKG changes in Figure A were in retrospect related to significant hyperkalemia with tachycardia, which coincided with the bladder pacemaker spikes causing the elusive appearance of dual chamber pacing with wide QRS rhythm and peaked T waves preceded by pacemaker spikes.
Discussion
EKG recording errors have been reported in approximately 6.5% of EKGs performed in a hospital setting [1]. Interference on an EKG from adjacent electrical devices has been reported previously not only in the setting of a bladder stimulation device [2], but also from a variety of extracardiac stimulators [3].
Many types of EKG artifacts have been reported [4] which include a several types of lead reversals or misplacements and tremor artifacts related to patient motion such as in Parkinson’s disease. Of greater than 1000 EKGs performed in a hospital setting, 5.9% were reported to have artifact, about 17% of which was AC noise (interference) artifact [5]. It is important to be vigilant of such artifacts [6] to avoid misinterpretation of these EKGs as cardiac arrhythmia or cardiac pacing (as in our case) and find ways to reduce such errors which can impact patient care [7].
References
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulikkumar Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The above electrocardiogram (EKG) in Figure A reveals pacemaker spikes preceding a wide QRS complex rhythm initially suggestive of dual chamber (AV sequential) pacing. Closer scrutiny (insert) reveals additional pacemaker spikes on the T waves which are inappropriate and do not support a pacing role for the detected spikes. Review of a prior EKG in Figure B revealed very fast pacing spikes with a cycle length of approximately 77 ms, and a rate of about 780/minute, thought to be AC interference (insert). The Chest X ray did not reveal evidence of any cardiac pacemaker. A Kidney, Ureter and Bladder (KUB) X ray, however, revealed a bladder pacemaker historically placed for atonic bladder as the cause for this interference artifact, likely set at 13 Hz, as seen in Figure C. The EKG changes in Figure A were in retrospect related to significant hyperkalemia with tachycardia, which coincided with the bladder pacemaker spikes causing the elusive appearance of dual chamber pacing with wide QRS rhythm and peaked T waves preceded by pacemaker spikes.
Discussion
EKG recording errors have been reported in approximately 6.5% of EKGs performed in a hospital setting [1]. Interference on an EKG from adjacent electrical devices has been reported previously not only in the setting of a bladder stimulation device [2], but also from a variety of extracardiac stimulators [3].
Many types of EKG artifacts have been reported [4] which include a several types of lead reversals or misplacements and tremor artifacts related to patient motion such as in Parkinson’s disease. Of greater than 1000 EKGs performed in a hospital setting, 5.9% were reported to have artifact, about 17% of which was AC noise (interference) artifact [5]. It is important to be vigilant of such artifacts [6] to avoid misinterpretation of these EKGs as cardiac arrhythmia or cardiac pacing (as in our case) and find ways to reduce such errors which can impact patient care [7].
References
- Moses A, Malozzi C, Omar B. Prevalence of ECG Recording Errors in a University Hospital ECG Database. Circ Cardiovasc Qual Outcomes. 2016 February;9:A236.
- Madias JE. Electrocardiographic artifact induced by an electrical stimulator implanted for management of neurogenic bladder. J Electrocardiol. 2008 Sep-Oct;41(5):401-3.
- Guinand A, Noble S, Frei A, Renard J, Tramer MR, Burri H. Extra-cardiac stimulators: what do cardiologists need to know? Europace. 2016 Sep;18(9):1299-307.
- Pérez-Riera AR, Barbosa-Barros R, Daminello-Raimundo R, de Abreu LC. Main artifacts in electrocardiography. Ann Noninvasive Electrocardiol. 2018 Mar;23(2):e12494.
- Awan MU, Omar M, Omar B, Malozzi C, Awan MU. ECG Recording Errors Prevalence in a Hospital Setting. Circ Cardiovasc Qual Outcomes. 2018 April; 2018;11:A244.
- Drew BJ. Pitfalls and artifacts in electrocardiography. Cardiol Clin. 2006 Aug;24(3):309-15, vii.
- Davies A. Recognizing and reducing interference on 12-lead electrocardiograms. Br J Nurs. 2007 Jul 12-25;16(13):800-4.
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulikkumar Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL