October 2020 Issue
ISSN 2689-291X
ISSN 2689-291X
Ebstein’s Anomaly.. Associated LV Noncompaction!
Description
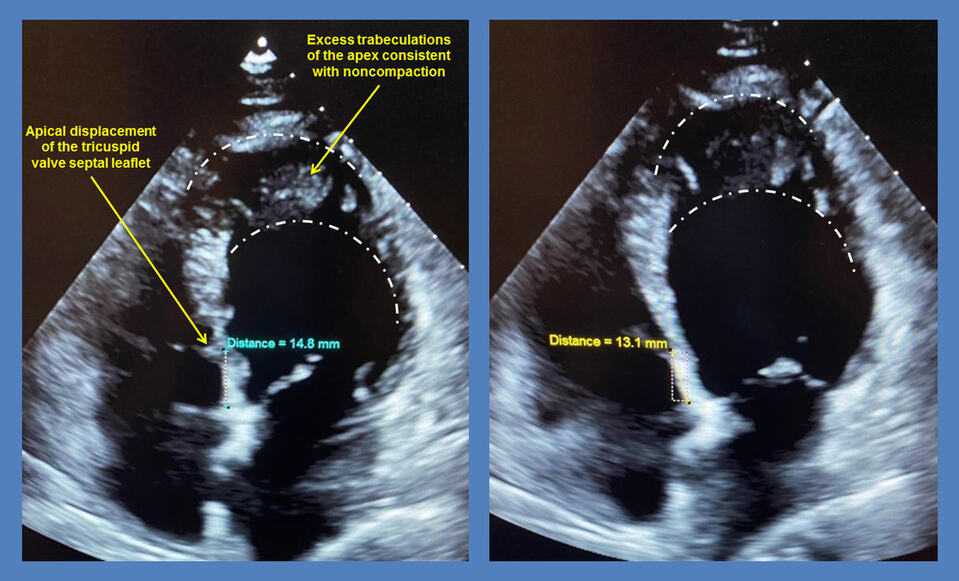
The above 2-dimensional (2-D) apical 4-chamber echocardiography images and the accompanying video clip demonstrate apical displacement of the tricuspid valve annulus (by > 8mm/m2 body surface area) with tethering of the septal leaflet to the left ventricular septum, associated with redundancy of the leaflets and atrialization of a portion of the right ventricle; all features diagnostic of Ebstein’s anomaly.
The left ventricular apex and lateral wall segments contain numerous prominent trabeculations with deep intertrabecular recesses, at least twice the thickness of the compacted wall, both in systole and diastole, which is highly suggestive of associated left ventricular noncompaction (LVNC). This condition is rarely associated with Ebstein’s anomaly.
Discussion:
Ebstein’s anomaly involves apical displacement of the tricuspid annulus due to tethering of the septal and posterior tricuspid valve leaflets to the underlying right ventricular septum and free wall, a rare congenital lesion found in approximately one of 200,000 live births [1]. This results in atrialization of the right ventricle as the apically displaced tricuspid valve leaflets encroach upon the right ventricular (RV) apex and outflow tract, causing RV dysfunction. Multi-modality imaging can help diagnose the extent of the functional abnormalities and associated lesions [2].
While two-dimensional (2-D) echocardiography remains the standard method of assessment in Ebstein’s anomaly [3], augmentation of the 2-D views with 3-D echocardiographic and transesophageal (TEE) imaging can provide important supplemental information about the extent of the functional abnormalities in addition to the presence and severity of associated anomalies or defects [4].
Ebstein’s anomaly is often associated with an atrial septal defect and right-sided accessory pathways (Wolff-Parkinson-White; WPW), which can cause stroke [6], palpitations [7] and may contribute to progressive dyspnea [8]. Successful percutaneous ASD closure [9] and WPW ablation [10] in patients with Ebstein’s anomaly have been reported.
Syndromic associations of Ebstein’s anomaly are quite rare, and add tremendously to the complexity of its diagnosis and management. Ebstein’s anomaly has been reported in association with Down’s syndrome [11] in addition to Tetralogy of Fallot and absent pulmonary valve syndrome [12]. Other associations include Williams syndrome [13] and congenitally corrected transposition of the great vessels [14]. Extracardiac manifestations have also been reported in association with Ebstein’s anomaly [15].
Another interesting association with Ebstein’s anomaly is noncompaction cardiomyopathy [16]. This may involve left ventricular noncompaction [17], right ventricular noncompaction [18] or biventricular noncompaction [19]. The original classification of isolated ventricular noncompaction by Jenni et al [20] entailed the presence of deep perfused intertrabecular recesses by color Doppler echocardiography predominantly in the mid-lateral, apical and mid-inferior segments with a noncompacted myocardium twice the compacted layer in systole, in the absence other coexisting abnormalities. Other classifications have been proposed since then [21] with realization of the need for early management goals based on left ventricular systolic function and secondary complications [22].
While multiple genetic mutations have been associated with each of Ebstein’s anomaly and noncompaction cardiomyopathy individually, the coexistence of both conditions together has been linked to genetic mutations involving the sarcomeric protein gene MYH7 [23] in addition to TPM1, encoding a-tropomyosin [24]. This combination appears to complicate the management of either condition individually and result in increased mortality [25].
References:
Mustafeez Ur Rahman, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Landai Nguyen, D.O.
Staff Cardiologist
The Heart Center of Northeast Georgia Medical Center,
Cumming, GA
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The above 2-dimensional (2-D) apical 4-chamber echocardiography images and the accompanying video clip demonstrate apical displacement of the tricuspid valve annulus (by > 8mm/m2 body surface area) with tethering of the septal leaflet to the left ventricular septum, associated with redundancy of the leaflets and atrialization of a portion of the right ventricle; all features diagnostic of Ebstein’s anomaly.
The left ventricular apex and lateral wall segments contain numerous prominent trabeculations with deep intertrabecular recesses, at least twice the thickness of the compacted wall, both in systole and diastole, which is highly suggestive of associated left ventricular noncompaction (LVNC). This condition is rarely associated with Ebstein’s anomaly.
Discussion:
Ebstein’s anomaly involves apical displacement of the tricuspid annulus due to tethering of the septal and posterior tricuspid valve leaflets to the underlying right ventricular septum and free wall, a rare congenital lesion found in approximately one of 200,000 live births [1]. This results in atrialization of the right ventricle as the apically displaced tricuspid valve leaflets encroach upon the right ventricular (RV) apex and outflow tract, causing RV dysfunction. Multi-modality imaging can help diagnose the extent of the functional abnormalities and associated lesions [2].
While two-dimensional (2-D) echocardiography remains the standard method of assessment in Ebstein’s anomaly [3], augmentation of the 2-D views with 3-D echocardiographic and transesophageal (TEE) imaging can provide important supplemental information about the extent of the functional abnormalities in addition to the presence and severity of associated anomalies or defects [4].
Ebstein’s anomaly is often associated with an atrial septal defect and right-sided accessory pathways (Wolff-Parkinson-White; WPW), which can cause stroke [6], palpitations [7] and may contribute to progressive dyspnea [8]. Successful percutaneous ASD closure [9] and WPW ablation [10] in patients with Ebstein’s anomaly have been reported.
Syndromic associations of Ebstein’s anomaly are quite rare, and add tremendously to the complexity of its diagnosis and management. Ebstein’s anomaly has been reported in association with Down’s syndrome [11] in addition to Tetralogy of Fallot and absent pulmonary valve syndrome [12]. Other associations include Williams syndrome [13] and congenitally corrected transposition of the great vessels [14]. Extracardiac manifestations have also been reported in association with Ebstein’s anomaly [15].
Another interesting association with Ebstein’s anomaly is noncompaction cardiomyopathy [16]. This may involve left ventricular noncompaction [17], right ventricular noncompaction [18] or biventricular noncompaction [19]. The original classification of isolated ventricular noncompaction by Jenni et al [20] entailed the presence of deep perfused intertrabecular recesses by color Doppler echocardiography predominantly in the mid-lateral, apical and mid-inferior segments with a noncompacted myocardium twice the compacted layer in systole, in the absence other coexisting abnormalities. Other classifications have been proposed since then [21] with realization of the need for early management goals based on left ventricular systolic function and secondary complications [22].
While multiple genetic mutations have been associated with each of Ebstein’s anomaly and noncompaction cardiomyopathy individually, the coexistence of both conditions together has been linked to genetic mutations involving the sarcomeric protein gene MYH7 [23] in addition to TPM1, encoding a-tropomyosin [24]. This combination appears to complicate the management of either condition individually and result in increased mortality [25].
References:
- Attenhofer Jost CH, Connolly HM, Dearani JA, Edwards WD, Danielson GK. Ebstein's anomaly. Circulation. 2007 Jan 16;115(2):277-85.
- Qureshi MY, O'Leary PW, Connolly HM. Cardiac imaging in Ebstein anomaly. Trends Cardiovasc Med. 2018 Aug;28(6):403-409.
- Oechslin E, Buchholz S, Jenni R. Ebstein's anomaly in adults: Doppler-echocardiographic evaluation. Thorac Cardiovasc Surg. 2000 Aug;48(4):209-13.
- Booker OJ, Nanda NC. Echocardiographic assessment of Ebstein's anomaly. Echocardiography. 2015 Jan;32 Suppl 2:S177-88.
- Hasan MN, Ahmed K, Ahmed SM, Rahman MM. Ebstein's Anomaly Associated with Atrial Septal Defect and Wolff-Parkinson-White (WPW) Syndrome. Mymensingh Med J. 2017 Jul;26(3):676-679.
- Tan NY, Attenhofer Jost CH, Polkinghorne MD, Vargas ER, Hodge DO, Dearani JA, Asirvatham SJ, Connolly HM, McLeod CJ. Cerebrovascular accidents in Ebstein's anomaly. Congenit Heart Dis. 2019 Nov;14(6):1157-1165.
- Marcu CB, Donohue TJ. A young man with palpitations and Ebstein's anomaly of the tricuspid valve. CMAJ. 2005 Jun 7;172(12):1553-4.
- Carrizales-Sepúlveda EF, Vera-Pineda R, Flores-Ramírez R, Ordaz-Farías A. A young male with progressive dyspnea: Ebstein's anomaly. Intern Emerg Med. 2019 Apr;14(3):489-490.
- Oka K, Seki M, Kataoka K, Sato T, Imai Y, Yamagata T. Percutaneous Atrial Septal Defect Closure in Adult Ebstein's Anomaly with Exertional Hypoxemia. Int Heart J. 2020 May 30;61(3):620-623.
- Gül EE, Akdeniz C, Tuzcu V. Successful ablation of coexistent Mahaim tachycardia and right posterior accessory pathway in a patient with Ebstein's anomaly. Turk Kardiyol Dern Ars. 2016 Jul;44(5):423-6.
- Pepeta L, Clur SA. Ebstein's anomaly and Down's syndrome. Cardiovasc J Afr. 2013 Oct-Nov;24(9-10):382-4.
- Abramian A, Gembruch U, Geipel A, Müller AM, Baier B, Berg C. Ebstein's anomaly of the tricuspid valve in association with Tetralogy of Fallot and absent pulmonary valve syndrome. Fetal Diagn Ther. 2011;30(2):153-6.
- Changela V, Maheshwari S, Bhat M. Williams syndrome and Ebstein's anomaly: A rare association. Ann Pediatr Cardiol. 2009 Jul;2(2):165-6.
- Henry JG, Gordon S, Timmis GC. Corrected transposition of great vessels and Ebstein's anomaly of tricuspid valve. Echocardiographic findings. Br Heart J. 1979 Feb;41(2):249-52.
- Siebert JR, Barr M Jr, Jackson JC, Benjamin DR. Ebstein's anomaly and extracardiac defects. Am J Dis Child. 1989 May;143(5):570-2.
- Attenhofer Jost CH, Connolly HM, Warnes CA, O'leary P, Tajik AJ, Pellikka PA, Seward JB. Noncompacted myocardium in Ebstein's anomaly: initial description in three patients. J Am Soc Echocardiogr. 2004 Jun;17(6):677-80.
- Bagur RH, Lederlin M, Montaudon M, Latrabe V, Corneloup O, Iriart X, Laurent F. Ebstein Anomaly Associated With Left Ventricular Noncompaction. Circulation. 2008;118:e662–e664
- Song ZZ. A combination of right ventricular hypertrabeculation/ noncompaction and Ebstein's anomaly. Int J Cardiol. 2010 Aug 20;143(2):e30-3.
- Fazio G, Visconti C, D'angelo L, Grassedonio E, Lo Re G, D'Amico T, Sutera L, Novo G, Ferrara F, Midiri M, Novo S. Diagnosis and definition of biventricular non-compaction associated to Ebstein's anomaly. Int J Cardiol. 2011 Jul 1;150(1):e20-4.
- Jenni R, Oechslin E, Schneider J, Attenhofer Jost C, Kaufmann PA. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart. 2001 Dec;86(6):666-71.
- Gati S, Rajani R, Carr-White GS, Chambers JB. Adult left ventricular noncompaction: reappraisal of current diagnostic imaging modalities. JACC Cardiovasc Imaging. 2014 Dec;7(12):1266-75.
- Bennett CE, Freudenberger R. The Current Approach to Diagnosis and Management of Left Ventricular Noncompaction Cardiomyopathy: Review of the Literature. Cardiol Res Pract. 2016;2016:5172308.
- Vermeer AM, van Engelen K, Postma AV, Baars MJ, Christiaans I, De Haij S, Klaassen S, Mulder BJ, Keavney B. Ebstein anomaly associated with left ventricular noncompaction: an autosomal dominant condition that can be caused by mutations in MYH7. Am J Med Genet C Semin Med Genet. 2013 Aug;163C(3):178-84.
- Nijak A, Alaerts M, Kuiperi C, Corveleyn A, Suys B, Paelinck B, Saenen J, Van Craenenbroeck E, Van Laer L, Loeys B, Verstraeten A. Left ventricular non-compaction with Ebstein anomaly attributed to a TPM1 mutation. Eur J Med Genet. 2018 Jan;61(1):8-10.
- McGee M, Warner L, Collins N. Ebstein's Anomaly, Left Ventricular Noncompaction, and Sudden Cardiac Death. Case Rep Cardiol. 2015;2015:854236.
Mustafeez Ur Rahman, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Landai Nguyen, D.O.
Staff Cardiologist
The Heart Center of Northeast Georgia Medical Center,
Cumming, GA
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL