October 2021 Issue
ISSN 2689-291X
ISSN 2689-291X
McGinn-White Sign..
S1Q3T3 Pattern of Acute Pulmonary Embolism!
Description
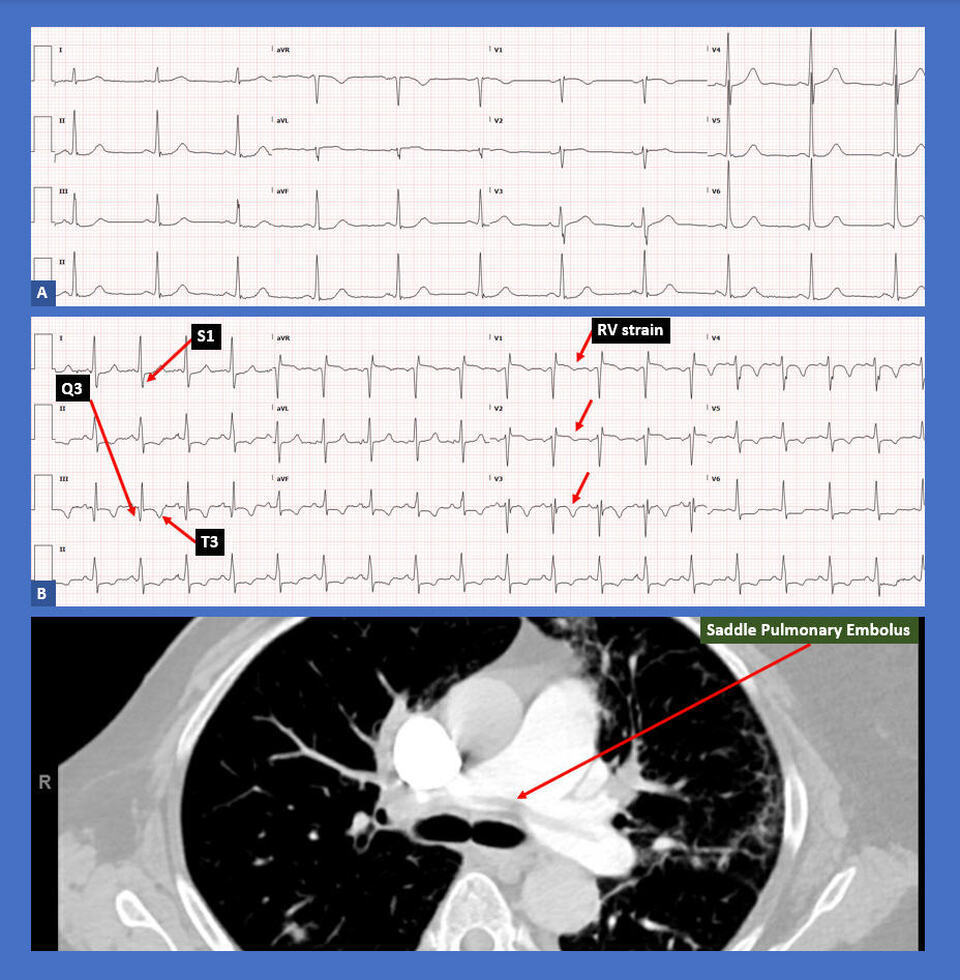
EKG A reveals normal sinus rhythm and is grossly within normal limits. EKG B, greater than 2 years since EKG A, was associated with a presentation of acute dyspnea and hypotension. It reveals sinus tachycardia, with a new appearance of a prominent S wave in lead I, a Q wave in lead III and T wave inversion in lead III (and diffusely) suggestive of acute right ventricular strain. The CT angiogram revealed a massive saddle pulmonary embolus which required immediate surgical embolectomy due to hemodynamic instability.
Discussion
The S1Q3T3 EKG pattern reflecting acute cor pulmonale, often resulting from acute pulmonary embolism, was first described in seven patients by Sylvester Mcginn and Paul White in 1935 [1]. The EKG pattern was attributed to the sudden dilatation of the right ventricle and right atrium.
Other associated findings on the EKG have been described as indicative of acute RV strain. ST elevation in lead aVR in addition to an S1Q3T3 pattern was reported in a patient with massive pulmonary embolism and hemoptysis [2].
Although several electrocardiographic signs of right heart strain have been described, in general the value of the EKG in establishing a diagnosis of pulmonary embolism remains limited. The EKG findings are often variable, overlap with other disease entities and temporary, limiting their usefulness [3].
S1Q3T3 pattern has been described in the setting of acute bronchospasm. Arshad et al. [4] reported this pattern in a 33 year old pregnant female with known asthma presenting with acute bronchospasm, other causes including pulmonary embolism, were excluded.
Sub-massive pulmonary embolism was reported in a 50 year old male presenting with acute anterior ST elevation myocardial infarction (STEMI) by Siddiqa et al. [5]. Following prompt coronary angiography negative for coronary artery disease, the diagnosis of pulmonary embolism was established by computed tomography angiography (CTA) of the chest and by deep vein thrombosis (DVT) demonstrated on lower extremity venous ultrasound.
EKG changes of RV strain following pulmonary embolism are expected to resolve following treatment, although some patients may be left with chronic cor pulmonale EKG changes, especially after repeated episodes. Spontaneous resolution of the S1Q3T3 pattern is rare and has been previously reported [6].
Supplementing EKG findings suggestive of acute coronary syndromes or pulmonary embolism with bedside echocardiography can be very helpful in the early differentiation of STEMI, pulmonary embolism or other diagnoses [7]. The McConnell’s sign on echocardiogram, although not very sensitive, has been reported to have up to 97% specificity for acute pulmonary embolism [8].
Daniel et al. [9] proposed a 21-point scoring system derived from the 12-lead EKG for the assessment of the severity of pulmonary hypertension in the setting of acute pulmonary embolism. The point system includes sinus tachycardia (2), incomplete RBBB (2), complete RBBB (3), inverted T-waves in V1 – V4 (0 – 12), S wave in lead I (0), Q wave in lead III (1), inverted T-wave in lead III (1), and entire S1Q3T3 complex (2). A score of 10 or greater is indicative of pulmonary embolism with severe pulmonary hypertension.
In conclusion, despite several pitfalls associated with the use of the EKG in the diagnosis of pulmonary embolism, combined electrocardiographic criteria, in addition to the traditional S1Q3T3 pattern, make it a useful tool for assessing the severity of the disease and for prognostication [10].
References:
Authors:
Alexis Parks, D.O.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
EKG A reveals normal sinus rhythm and is grossly within normal limits. EKG B, greater than 2 years since EKG A, was associated with a presentation of acute dyspnea and hypotension. It reveals sinus tachycardia, with a new appearance of a prominent S wave in lead I, a Q wave in lead III and T wave inversion in lead III (and diffusely) suggestive of acute right ventricular strain. The CT angiogram revealed a massive saddle pulmonary embolus which required immediate surgical embolectomy due to hemodynamic instability.
Discussion
The S1Q3T3 EKG pattern reflecting acute cor pulmonale, often resulting from acute pulmonary embolism, was first described in seven patients by Sylvester Mcginn and Paul White in 1935 [1]. The EKG pattern was attributed to the sudden dilatation of the right ventricle and right atrium.
Other associated findings on the EKG have been described as indicative of acute RV strain. ST elevation in lead aVR in addition to an S1Q3T3 pattern was reported in a patient with massive pulmonary embolism and hemoptysis [2].
Although several electrocardiographic signs of right heart strain have been described, in general the value of the EKG in establishing a diagnosis of pulmonary embolism remains limited. The EKG findings are often variable, overlap with other disease entities and temporary, limiting their usefulness [3].
S1Q3T3 pattern has been described in the setting of acute bronchospasm. Arshad et al. [4] reported this pattern in a 33 year old pregnant female with known asthma presenting with acute bronchospasm, other causes including pulmonary embolism, were excluded.
Sub-massive pulmonary embolism was reported in a 50 year old male presenting with acute anterior ST elevation myocardial infarction (STEMI) by Siddiqa et al. [5]. Following prompt coronary angiography negative for coronary artery disease, the diagnosis of pulmonary embolism was established by computed tomography angiography (CTA) of the chest and by deep vein thrombosis (DVT) demonstrated on lower extremity venous ultrasound.
EKG changes of RV strain following pulmonary embolism are expected to resolve following treatment, although some patients may be left with chronic cor pulmonale EKG changes, especially after repeated episodes. Spontaneous resolution of the S1Q3T3 pattern is rare and has been previously reported [6].
Supplementing EKG findings suggestive of acute coronary syndromes or pulmonary embolism with bedside echocardiography can be very helpful in the early differentiation of STEMI, pulmonary embolism or other diagnoses [7]. The McConnell’s sign on echocardiogram, although not very sensitive, has been reported to have up to 97% specificity for acute pulmonary embolism [8].
Daniel et al. [9] proposed a 21-point scoring system derived from the 12-lead EKG for the assessment of the severity of pulmonary hypertension in the setting of acute pulmonary embolism. The point system includes sinus tachycardia (2), incomplete RBBB (2), complete RBBB (3), inverted T-waves in V1 – V4 (0 – 12), S wave in lead I (0), Q wave in lead III (1), inverted T-wave in lead III (1), and entire S1Q3T3 complex (2). A score of 10 or greater is indicative of pulmonary embolism with severe pulmonary hypertension.
In conclusion, despite several pitfalls associated with the use of the EKG in the diagnosis of pulmonary embolism, combined electrocardiographic criteria, in addition to the traditional S1Q3T3 pattern, make it a useful tool for assessing the severity of the disease and for prognostication [10].
References:
- Mcginn S, White P. Acute Cor Pulmonale Resulting From Pulmonary Embolism: Its Clinical Recognition. JAMA. 1935;104(17):1473-1480.
- Islamoglu MS, Dokur M, Ozdemir E, Unal OF. Massive pulmonary embolism presenting with hemoptysis and S1Q3T3 ECG findings. BMC Cardiovasc Disord. 2021 May 1;21(1):224.
- Chan TC, Vilke GM, Pollack M, Brady WJ. Electrocardiographic manifestations: pulmonary embolism. J Emerg Med. 2001 Oct;21(3):263-70.
- Arshad H, Khan RR, Khaja M. Case Report of S1Q3T3 Electrocardiographic Abnormality in a Pregnant Asthmatic Patient During Acute Bronchospasm. Am J Case Rep. 2017 Feb 1;18:110-113.
- Siddiqa A, Haider A, Jog A, Yue B, Krim NR. Pulmonary Embolism Presenting as ST-Elevation Myocardial Infarction: A Diagnostic Trap. Am J Case Rep. 2020 Nov 28;21:e927923.
- Cygan LD, Weizberg M, Hahn B. Spontaneous, resolving S1Q3T3 in pulmonary embolism: A case report and literature review on prognostic value of electrocardiography score for pulmonary embolism. Int Emerg Nurs. 2016 Sep;28:46-9.
- Chamsi-Pasha MA, Aljaroudi W, Alraiyes AH, Alraies MC. McConnell sign and S1Q3T3 pattern in pulmonary embolism: revisited. BMJ Case Rep. 2013 May 13;2013:bcr2013009623.
- Andrews A, Malone K, Omar B. McConnell’s Sign.. RV Strain in Acute Pulmonary Embolism! Cardiofel Newslet 2021 Jan; 4(1):1– 3.
- Daniel KR, Courtney DM, Kline JA. Assessment of cardiac stress from massive pulmonary embolism with 12-lead ECG. Chest. 2001 Aug;120(2):474-81.
- Digby GC, Kukla P, Zhan ZQ, Pastore CA, Piotrowicz R, Schapachnik E, Zareba W, Bayés de Luna A, Pruszczyk P, Baranchuk AM. The value of electrocardiographic abnormalities in the prognosis of pulmonary embolism: a consensus paper. Ann Noninvasive Electrocardiol. 2015 May;20(3):207-23.
Authors:
Alexis Parks, D.O.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL