October 2019 Issue
ISSN 2689-291X
ISSN 2689-291X
Challenging Images
Inadvertent Subclavian Artery Canulation..The Tip Is In The Tip!
Description
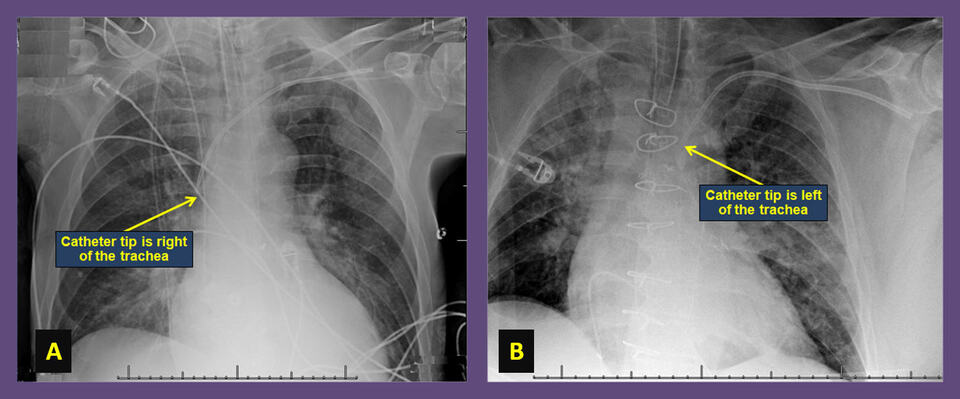
The chest x-rays (CXR) shown were taken to confirm central venous line position and rule out pneumothorax in two different patients, using a left subclavian vein access. Both revealed no pneumothorax. The CXR on the left (A) demonstrates a normal course of the catheter with the tip ending on the right of the trachea where the right atrium is expected. The CXR on the right (B), however, exhibits an atypical course of the catheter with the tip ending on the left side of the trachea, indicating a possible inadvertent canulation of the left subclavian artery, which was confirmed with pressure transduction.
Central venous catheters provide an easy and reliable access to the venous circulation for administration of medications and hemodynamic measurements in the critically ill patient, and have been in use for many decades [1]. The most common access sites include the internal jugular, subclavian and femoral veins; all of which run alongside their corresponding arteries, which pauses a risk of inadvertent arterial canulation and injury [2].
The overall reported complication rate with central venous access is 14%; including arterial puncture, improper position, pneumothorax, hematoma, hemothorax, and asystolic cardiac arrest of unknown etiology; with the subclavian approach accounting for the greatest percentage (39%) of observed complications [3]. The subclavian vein approach is particularly susceptible to unintentional artery canulation due to the depth of the vein underneath the clavicle and the difficulty using ultrasound guidance; this complication has been reported in 2.7% of subclavian vein approach procedures, compared to 1% for the internal jugular vein technique [4].
Musculoskeletal abnormalities, anomalous vascular anatomy, hypotension causing loss of pulsatile flow and emergent nature of the procedure can increase the risk of arterial canulation. Stroke [5] and subclavian artery occlusion during endovascular repair of such arterial injuries [6] have been reported.
Prompt recognition of iatrogenic arterial injury is crucial to early successful repair. Catheter tip position on CXR and transduction of an arterial waveform can confirm the diagnosis. CT scan of the chest and angiography help assess the extent of the injury and identify an entry site [7].
Successful endovascular repair of subclavian artery canulation injury has been reported utilizing collagen-based closure devices (Angioseal) [8], suture-mediated closure devices (Perclose) [9], temporary balloon tamponade [10], stent–graft placement [11], Gelfoam Pledget tract embolization and gradual sheath downsizing [12]. Manual compression is rarely sufficient given the lack of compressibility of the vessel, and may cause a pseudoaneurysm or a massive hemothorax.
References:
Authors:
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The chest x-rays (CXR) shown were taken to confirm central venous line position and rule out pneumothorax in two different patients, using a left subclavian vein access. Both revealed no pneumothorax. The CXR on the left (A) demonstrates a normal course of the catheter with the tip ending on the right of the trachea where the right atrium is expected. The CXR on the right (B), however, exhibits an atypical course of the catheter with the tip ending on the left side of the trachea, indicating a possible inadvertent canulation of the left subclavian artery, which was confirmed with pressure transduction.
Central venous catheters provide an easy and reliable access to the venous circulation for administration of medications and hemodynamic measurements in the critically ill patient, and have been in use for many decades [1]. The most common access sites include the internal jugular, subclavian and femoral veins; all of which run alongside their corresponding arteries, which pauses a risk of inadvertent arterial canulation and injury [2].
The overall reported complication rate with central venous access is 14%; including arterial puncture, improper position, pneumothorax, hematoma, hemothorax, and asystolic cardiac arrest of unknown etiology; with the subclavian approach accounting for the greatest percentage (39%) of observed complications [3]. The subclavian vein approach is particularly susceptible to unintentional artery canulation due to the depth of the vein underneath the clavicle and the difficulty using ultrasound guidance; this complication has been reported in 2.7% of subclavian vein approach procedures, compared to 1% for the internal jugular vein technique [4].
Musculoskeletal abnormalities, anomalous vascular anatomy, hypotension causing loss of pulsatile flow and emergent nature of the procedure can increase the risk of arterial canulation. Stroke [5] and subclavian artery occlusion during endovascular repair of such arterial injuries [6] have been reported.
Prompt recognition of iatrogenic arterial injury is crucial to early successful repair. Catheter tip position on CXR and transduction of an arterial waveform can confirm the diagnosis. CT scan of the chest and angiography help assess the extent of the injury and identify an entry site [7].
Successful endovascular repair of subclavian artery canulation injury has been reported utilizing collagen-based closure devices (Angioseal) [8], suture-mediated closure devices (Perclose) [9], temporary balloon tamponade [10], stent–graft placement [11], Gelfoam Pledget tract embolization and gradual sheath downsizing [12]. Manual compression is rarely sufficient given the lack of compressibility of the vessel, and may cause a pseudoaneurysm or a massive hemothorax.
References:
- Agee KR, Balk RA. Central venous catheterization in the critically ill patient. Crit Care Clin. 1992 Oct;8(4):677-86.
- Patel RY, Friedman A, Shams JN, et al. Central venous catheter tip malposition. J Med Imaging Radiat Oncol. 2010 Feb;54(1):35-42.
- Eisen LA, Narasimhan M, Berger JS, et al. Mechanical complications of central venous catheters. J Intensive Care Med. 2006 Jan-Feb;21(1):40-6.
- Iovino F1, Pittiruti M, Buononato M, et al. [Central venous catheterization: complications of different placements]. [Article in French]. Ann Chir. 2001 Dec;126(10):1001-6.
- Jahromi BS, Tummala RP, Levy EI. Inadvertent subclavian artery catheter placement complicated by stroke: endovascular management and review. Catheter Cardiovasc Interv. 2009 Apr 1;73(5):706-11.
- Sharma M, Sakhuja R, Teitel D, et al. Percutaneous arterial closure for inadvertent cannulation of the subclavian artery--a call for caution. J Invasive Cardiol. 2008 Jul;20(7):E229-32.
- Yoon DY, Annambhotla S, Resnick SA, et al. Inadvertent Arterial Placement of Central Venous Catheters: Diagnostic and Therapeutic Strategies. Ann Vasc Surg. 2015 Nov;29(8):1567-74.
- Ananthakrishnan G, White RD, Bhat R, et al. Inadvertent Subclavian Artery Cannulation: Endovascular Repair Using a Collagen Closure Device—Report of Two Cases and Review of the Literature. Case Rep Vasc Med. 2012; 2012: 150343.
- Chivate RS, Kulkarni SS, Shetty NS, et al. Percutaneous repair of iatrogenic subclavian artery injury by suture-mediated closure device. Indian J Radiol Imaging. 2016 Apr-Jun;26(2):262-6.
- Yu H, Stavas JM, Dixon RG, et. Temporary balloon tamponade for managing subclavian arterial injury by inadvertent central venous catheter placement. J Vasc Interv Radiol. 2011 May;22(5):654-9.
- Burbridge B, Stoneham G, Szkup P. Percutaneous subclavian artery stent-graft placement following failed ultrasound guided subclavian venous access. BMC Med Imaging. 2006 May 5;6:3.
- Abi-Jaoudeh N, Turba UC, Arslan B, et al. Management of subclavian arteral injuries following inadvertent arterial puncture during central venous catheter placement. J Vasc Interv Radiol. 2009 Mar;20(3):396-402.
Authors:
Sarina Sachdev, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL