October 2022 Issue
ISSN 2689-291X
ISSN 2689-291X
Paradoxical Embolism:
Cryptogenic Stroke Culprit!
Description
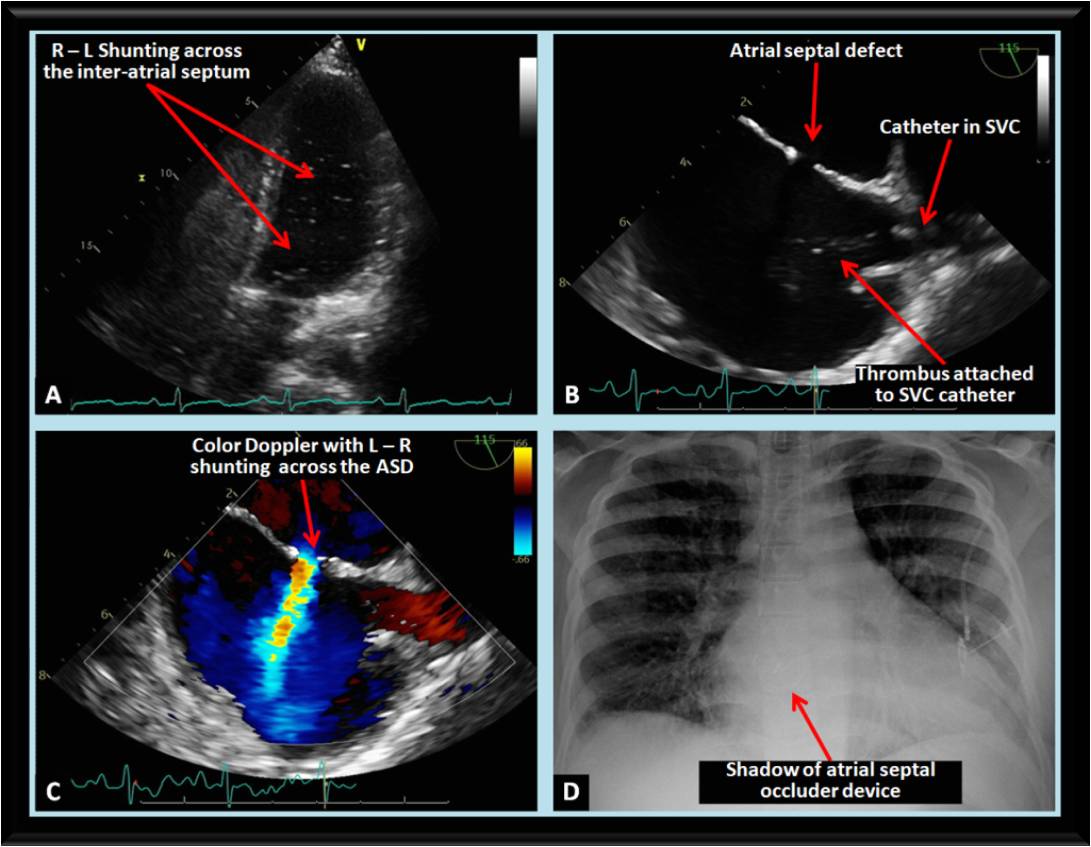
The above images were obtained on a patient undergoing work-up for stroke. Cardiomegaly was noted on chest roentgenogram (CXR). Transthoracic echocardiogram (TTE) revealed normal left ventricular size and systolic function and dilated right heart chambers. This prompted doing intravenous bubble contrast study which revealed spontaneous right to left (R – L) shunting across the interatrial septum (Figure A). Trasesophageal echocardiogram (TEE) (Figure B) revealed a 0.9 cm ostium secundum atrial septal defect (ASD) with left to right (L – R) shunting on color flow Doppler (Figure C). A catheter, placed for medication administration few months earlier, is also visualized within the superior vena cava (SVC) with an adherent thrombus, likely the cause of stroke due to paradoxical embolization across the ASD. Following anticoagulation with heparin and reported disappearance of the thrombus, a Gore Cardioform ASD occluder device was deployed successfully as shown on the follow-up CXR (Figure D).
Discussion
The interatrial septum starts forming during the fifth week of gestation, with potential for developmental abnormalities at the level of the endocardial cushion causing ostium primum ASD, at the level of the fossa ovalis causing ostium secundum ASD (> 80% of ASDs), or lack of fusion of the flap valve into the septum secundum which may result in a patent foramen ovale (PFO) [1].
ASDs are the most common form of congenital heart disease in the adult and pose a diagnostic and therapeutic challenge due to variable morphologies and presentations including right-sided heart failure, tachyarrhythmia, and embolic phenomena [2]. Iatrogenic ASDs (iASDs) are increasingly encountered since the advent of structural therapeutics requiring crossing the interatrial septum. The prevalence is likely related to the size and number of catheters used, and has been reported as 41% following mitral valve trascatheter edge-to-edge repair [3] and 20% following cryoablation pulmonary vein isolation for atrial fibrillation [4].
PFO has long been associated with cryptogenic stroke, especially in the presence of an atrial septal aneurysm [5]. PFO closure may help reduce stroke, however evidence of its effectiveness and safety compared with contemporary medical therapy is lacking [6]. The 2021 American Heart Association/American Stroke Association guideline for the prevention of stroke in patients with stroke or transient ischemia attack [7] gives a reasonable indication (Class 2a) for PFO closure and long term antiplatelet therapy in patients 18 – 60 years old with nonlacunar ischemic infarct of unknown cause and high-risk PFO (presence of atrial septal aneurysm or large right to left shunt).
Attention should be paid to the potential presence of simultaneous extracardiac shunting while evaluating an ASD or a PFO. A reported case of paradoxical embolism in the presence of a PFO revealed residual shunting following PFO closure, identified to be through a pulmonary arterio-venous malformation, which required subsequent embolization for successful control of symptoms [8].
Echocardiograpy, both TTE and TEE, remains the mainstay of the diagnosis and characterization of a PFO to allow assessment of its paradoxical embolism potential, any other associated anomalies and plan definitive treatment [9]. Three-dimensional TEE provides further delineation of a paradoxical embolus in both atria while in transit [10]. Multimodality imaging using computed tomography (CT), magnetic resonance imaging (MRI), peripheral venous and transcranial Doppler ultrasound are essential in the detection of embolic sources, intracardiac versus extracardiac shunting, and vascular disease [11].
The presence of deep vein thrombosis (DVT) and/ or pulmonary embolism together with an arterial embolus raises suspicion for paradoxical embolism [12]. The extent of the embolism can be significant and may involve all cardiac chambers [13]. In the presence of massive pulmonary embolism requiring pulmonary embolectomy, simultaneous surgical closure of a PFO should be considered [14].
Occasionally paradoxical embolism can originate from other thrombotic sources than DVT, such as venous or right atrial devices or catheters [15], as is evident from the case discussed above. The route of paradoxical embolism in certain cases may not involve a PFO or an ASD, and can be through large pulmonary arteriovenous malformations [16], which may require coil embolization closure.
Embolic material can occasionally by friable tumor tissue such as intravenous leiomyomatosis extending from a uterine leiomyoma [17], rather than thrombotic material. Gas embolization has also been reported to cause paradoxical embolism, across presumed extracardiac shunting through the pulmonary circulation, during surgical hyseteroscopy [18]. Similarly, paradoxical embolization has been reported following endoscopic carbon dioxide gas insufflation during endoscopic thyroidectomy, presumably through an extracardiac transpulmonary right to left shunt [19]. Prompt diagnosis and treatment is necessary in these cases as significant hemodynamic instability may occur.
Cryptogenic stroke in the presence of a PFO remains a clinical dilemma. Given the wide prevalence of PFO in the general population, it may be an incidental finding during the diagnostic work-up of stroke. An index incorporating multiple clinical criteria has been proposed to help identify a PFO as a cause of paradoxical embolism and cryptogenic stroke [20], therefore likely benefiting from closure. PFO and ASD closure techniques have come long ways with the advent of less invasive and relatively safe percutaneous devices. Although rare, atrial wall and aortic wall erosion remain a potentially lethal complication of such devices which requires prompt recognition [21].
In conclusion, paradoxical embolism is a heterogeneous and complex phenomenon which often requires a high index of suspicion and multimodality imaging techniques to elucidate the underlying pathology including the type of embolic material, route of shunting, and the end organ involved [22]. This will help devise the optimal treatment modality which may include observation, antiplatelet or anticoagulant therapy, percutaneous intervention including coil embolization of areteriovenous shunts and closure devices for intracardiac shunts, or surgical intervention.
References
Authors:
Arcole Brandon, B.S.
Medical Student
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The above images were obtained on a patient undergoing work-up for stroke. Cardiomegaly was noted on chest roentgenogram (CXR). Transthoracic echocardiogram (TTE) revealed normal left ventricular size and systolic function and dilated right heart chambers. This prompted doing intravenous bubble contrast study which revealed spontaneous right to left (R – L) shunting across the interatrial septum (Figure A). Trasesophageal echocardiogram (TEE) (Figure B) revealed a 0.9 cm ostium secundum atrial septal defect (ASD) with left to right (L – R) shunting on color flow Doppler (Figure C). A catheter, placed for medication administration few months earlier, is also visualized within the superior vena cava (SVC) with an adherent thrombus, likely the cause of stroke due to paradoxical embolization across the ASD. Following anticoagulation with heparin and reported disappearance of the thrombus, a Gore Cardioform ASD occluder device was deployed successfully as shown on the follow-up CXR (Figure D).
Discussion
The interatrial septum starts forming during the fifth week of gestation, with potential for developmental abnormalities at the level of the endocardial cushion causing ostium primum ASD, at the level of the fossa ovalis causing ostium secundum ASD (> 80% of ASDs), or lack of fusion of the flap valve into the septum secundum which may result in a patent foramen ovale (PFO) [1].
ASDs are the most common form of congenital heart disease in the adult and pose a diagnostic and therapeutic challenge due to variable morphologies and presentations including right-sided heart failure, tachyarrhythmia, and embolic phenomena [2]. Iatrogenic ASDs (iASDs) are increasingly encountered since the advent of structural therapeutics requiring crossing the interatrial septum. The prevalence is likely related to the size and number of catheters used, and has been reported as 41% following mitral valve trascatheter edge-to-edge repair [3] and 20% following cryoablation pulmonary vein isolation for atrial fibrillation [4].
PFO has long been associated with cryptogenic stroke, especially in the presence of an atrial septal aneurysm [5]. PFO closure may help reduce stroke, however evidence of its effectiveness and safety compared with contemporary medical therapy is lacking [6]. The 2021 American Heart Association/American Stroke Association guideline for the prevention of stroke in patients with stroke or transient ischemia attack [7] gives a reasonable indication (Class 2a) for PFO closure and long term antiplatelet therapy in patients 18 – 60 years old with nonlacunar ischemic infarct of unknown cause and high-risk PFO (presence of atrial septal aneurysm or large right to left shunt).
Attention should be paid to the potential presence of simultaneous extracardiac shunting while evaluating an ASD or a PFO. A reported case of paradoxical embolism in the presence of a PFO revealed residual shunting following PFO closure, identified to be through a pulmonary arterio-venous malformation, which required subsequent embolization for successful control of symptoms [8].
Echocardiograpy, both TTE and TEE, remains the mainstay of the diagnosis and characterization of a PFO to allow assessment of its paradoxical embolism potential, any other associated anomalies and plan definitive treatment [9]. Three-dimensional TEE provides further delineation of a paradoxical embolus in both atria while in transit [10]. Multimodality imaging using computed tomography (CT), magnetic resonance imaging (MRI), peripheral venous and transcranial Doppler ultrasound are essential in the detection of embolic sources, intracardiac versus extracardiac shunting, and vascular disease [11].
The presence of deep vein thrombosis (DVT) and/ or pulmonary embolism together with an arterial embolus raises suspicion for paradoxical embolism [12]. The extent of the embolism can be significant and may involve all cardiac chambers [13]. In the presence of massive pulmonary embolism requiring pulmonary embolectomy, simultaneous surgical closure of a PFO should be considered [14].
Occasionally paradoxical embolism can originate from other thrombotic sources than DVT, such as venous or right atrial devices or catheters [15], as is evident from the case discussed above. The route of paradoxical embolism in certain cases may not involve a PFO or an ASD, and can be through large pulmonary arteriovenous malformations [16], which may require coil embolization closure.
Embolic material can occasionally by friable tumor tissue such as intravenous leiomyomatosis extending from a uterine leiomyoma [17], rather than thrombotic material. Gas embolization has also been reported to cause paradoxical embolism, across presumed extracardiac shunting through the pulmonary circulation, during surgical hyseteroscopy [18]. Similarly, paradoxical embolization has been reported following endoscopic carbon dioxide gas insufflation during endoscopic thyroidectomy, presumably through an extracardiac transpulmonary right to left shunt [19]. Prompt diagnosis and treatment is necessary in these cases as significant hemodynamic instability may occur.
Cryptogenic stroke in the presence of a PFO remains a clinical dilemma. Given the wide prevalence of PFO in the general population, it may be an incidental finding during the diagnostic work-up of stroke. An index incorporating multiple clinical criteria has been proposed to help identify a PFO as a cause of paradoxical embolism and cryptogenic stroke [20], therefore likely benefiting from closure. PFO and ASD closure techniques have come long ways with the advent of less invasive and relatively safe percutaneous devices. Although rare, atrial wall and aortic wall erosion remain a potentially lethal complication of such devices which requires prompt recognition [21].
In conclusion, paradoxical embolism is a heterogeneous and complex phenomenon which often requires a high index of suspicion and multimodality imaging techniques to elucidate the underlying pathology including the type of embolic material, route of shunting, and the end organ involved [22]. This will help devise the optimal treatment modality which may include observation, antiplatelet or anticoagulant therapy, percutaneous intervention including coil embolization of areteriovenous shunts and closure devices for intracardiac shunts, or surgical intervention.
References
- Rojas CA, El-Sherief A, Medina HM, et al. Embryology and developmental defects of the interatrial septum. AJR Am J Roentgenol. 2010 Nov;195(5):1100-4.
- Brida M, Chessa M, Celermajer D, et al. Atrial septal defect in adulthood: a new paradigm for congenital heart disease. Eur Heart J. 2022 Jul 21;43(28):2660-2671.
- Paukovitsch M, Schneider LM, Reichart C, et al. Prevalence of iatrogenic atrial septal defects (iASD) after mitral valve (MV) transcatheter edge-to-edge repair (TEER) in the long-term follow-up. Open Heart. 2021 Oct;8(2):e001732.
- Chan NY, Choy CC, Yuen HC, et al. A Very Long-term Longitudinal Study on the Evolution and Clinical Outcomes of Persistent Iatrogenic Atrial Septal Defect After Cryoballoon Ablation. Can J Cardiol. 2019 Apr;35(4):396-404.
- Handke M, Harloff A, Olschewski M, et al. Patent foramen ovale and cryptogenic stroke in older patients. N Engl J Med. 2007 Nov 29;357(22):2262-8.
- Thaler A, Kvernland A, Kelly S, et al. Stroke Prevention in Patients with Patent Foramen Ovale. Curr Cardiol Rep. 2021 Oct 30;23(12):183.
- Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke. 2021 Jul;52(7):e364-e467.
- Nightingale S, Ray GS. Paradoxical embolism causing stroke and migraine. J Postgrad Med. 2010 Jul-Sep;56(3):206-8.
- Aggeli C, Verveniotis A, Andrikopoulou E, et al. Echocardiographic features of PFOs and paradoxical embolism: a complicated puzzle. Int J Cardiovasc Imaging. 2018 Dec;34(12):1849-1861.
- Cheng HL, Huang CH, Wang MJ, et al. Biatrial paradoxical embolism identified by three-dimensional transesophageal echocardiography. Ann Thorac Surg. 2013 Jun;95(6):2184.
- Saremi F, Emmanuel N, Wu PF, et al. Paradoxical embolism: role of imaging in diagnosis and treatment planning. Radiographics. 2014 Oct;34(6):1571-92.
- Guo S, Roberts I, Missri J. Paradoxical embolism, deep vein thrombosis, pulmonary embolism in a patient with patent foramen ovale: a case report. J Med Case Rep. 2007 Sep 25;1:104.
- Meacham RR 3rd, Headley AS, Bronze MS, et al. Impending paradoxical embolism. Arch Intern Med. 1998 Mar 9;158(5):438-48.
- Maron BA, Shekar PS, Goldhaber SZ. Paradoxical embolism. Circulation. 2010 Nov 9;122(19):1968-72.
- Di Stefano V, Di Fulvio M, Di Liberato L, et al. Paradoxical embolism through a patent foramen ovale from central venous catheter thrombosis: A potential cause of stroke. J Neurol Sci. 2020 Jul 15;414:116820.
- Cappa R, Du J, Carrera JF, et al. Ischemic Stroke Secondary to Paradoxical Embolism Through a Pulmonary Arteriovenous Malformation: Case Report and Review of the Literature. J Stroke Cerebrovasc Dis. 2018 Jul;27(7):e125-e127.
- Kong LY, Chen LL, Xiang W, et al. Intravenous Leiomyomatosis With Paradoxical Embolism: Unusual Presentation of Uterine Leiomyoma. Circ Cardiovasc Imaging. 2020 Jan;13(1):e009930.
- Rademaker BM, Groenman FA, van der Wouw PA, et al. Paradoxical gas embolism by transpulmonary passage of venous emboli during hysteroscopic surgery: a case report and discussion. Br J Anaesth. 2008 Aug;101(2):230-3.
- Kim SH, Park KS, Shin HY, et al. Paradoxical carbon dioxide embolism during endoscopic thyroidectomy confirmed by transesophageal echocardiography. J Anesth. 2010 Oct;24(5):774-7.
- Kent DM, Ruthazer R, Weimar C, et al. An index to identify stroke-related vs incidental patent foramen ovale in cryptogenic stroke. Neurology. 2013 Aug 13;81(7):619-25.
- Crawford GB, Brindis RG, Krucoff MW, et al. Percutaneous atrial septal occluder devices and cardiac erosion: a review of the literature. Catheter Cardiovasc Interv. 2012 Aug 1;80(2):157-67.
- Windecker S, Stortecky S, Meier B. Paradoxical embolism. J Am Coll Cardiol. 2014 Jul 29;64(4):403-15.
Authors:
Arcole Brandon, B.S.
Medical Student
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL