October 2024 Issue
ISSN 2689-291X
ISSN 2689-291X
Invisible Pacing Spikes: Pseudo LBBB!
Description
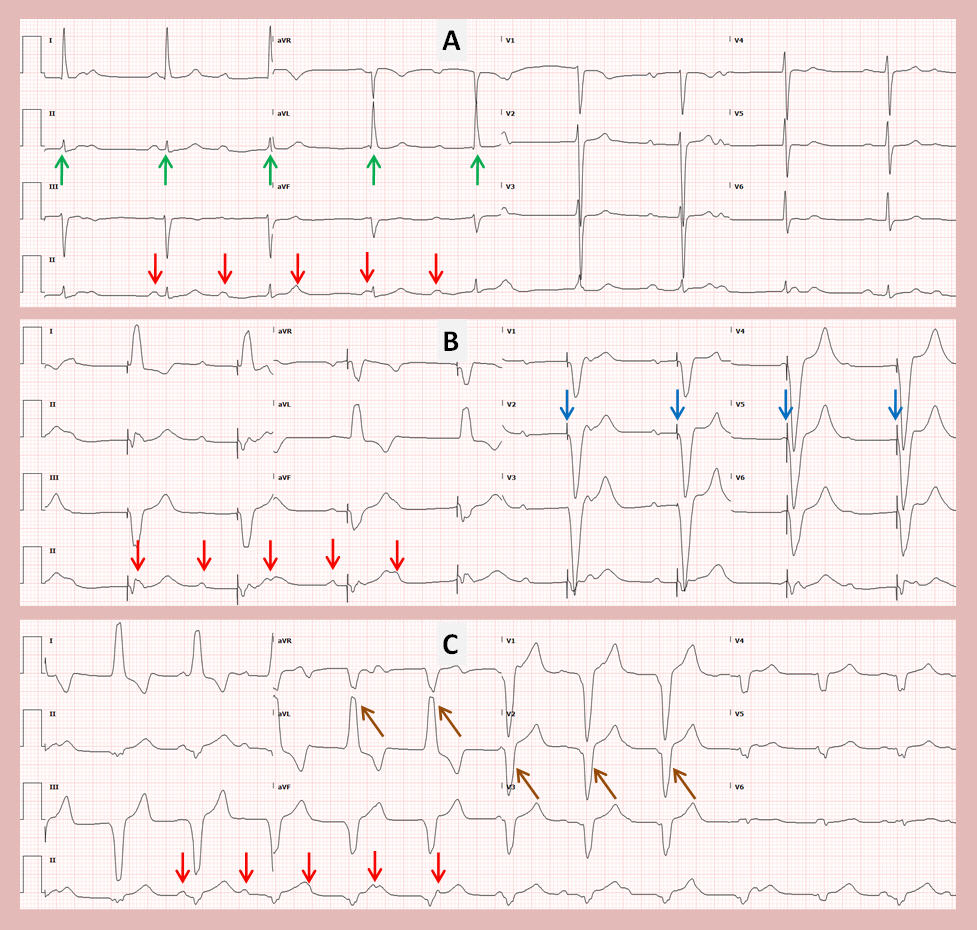
The above electrocardiograms (ECGs) reveal a case of complete heart block (CHB), with the P waves indicated by red arrows. Figure A reveals CHB with junctional escape beats (green arrows) at 53 beats per minute (BPM) and completed AV dissociation. Figure B shows temporary transvenous demand pacing at 50
BPM with manifest pacing spikes preceding paced complexes (blue arrows). Figure C, following insertion of a single-lead epicardial pacemaker, shows demand ventricular pacing at 70 BPM with paced beats lacking pacer spikes (brown arrows) and mimicking left bundle branch block (LBBB).
Discussion
Device implantation in general and pacemakers in particular, have gained widespread use due to a multitude of indications aimed at decreasing morbidity and mortality [1]. Traditionally a pacemaker consists of wires inserted through the left subclavian vein attached at one end to a generator implanted in the left upper chest wall while the distal end is fixed to the cardiac chamber intended to be paced. Variations to this, due to anatomic or infectious causes, include right-sided generator insertion [2], epicardial pacing [3], as in the images shown above, or leadless pacemakers [4].
It is imperative to be familiar with paced ECG interpretation to be able to troubleshoot pacemakers [5]. The absence of visible pacemaker spikes, as shown in the above discussed ECGs, does not exclude pacing [6]. Several factors can interfere with the amplitude of the pacemaker spike including the type of pacemaker, such as endocardial, epicardial or leadless; the mode of pacing, such as bipolar versus unipolar pacing; the pacing voltage, and other patient factors which may decrease the overall ECG signal including obesity, emphysema and anasarca [7].
References
The above electrocardiograms (ECGs) reveal a case of complete heart block (CHB), with the P waves indicated by red arrows. Figure A reveals CHB with junctional escape beats (green arrows) at 53 beats per minute (BPM) and completed AV dissociation. Figure B shows temporary transvenous demand pacing at 50
BPM with manifest pacing spikes preceding paced complexes (blue arrows). Figure C, following insertion of a single-lead epicardial pacemaker, shows demand ventricular pacing at 70 BPM with paced beats lacking pacer spikes (brown arrows) and mimicking left bundle branch block (LBBB).
Discussion
Device implantation in general and pacemakers in particular, have gained widespread use due to a multitude of indications aimed at decreasing morbidity and mortality [1]. Traditionally a pacemaker consists of wires inserted through the left subclavian vein attached at one end to a generator implanted in the left upper chest wall while the distal end is fixed to the cardiac chamber intended to be paced. Variations to this, due to anatomic or infectious causes, include right-sided generator insertion [2], epicardial pacing [3], as in the images shown above, or leadless pacemakers [4].
It is imperative to be familiar with paced ECG interpretation to be able to troubleshoot pacemakers [5]. The absence of visible pacemaker spikes, as shown in the above discussed ECGs, does not exclude pacing [6]. Several factors can interfere with the amplitude of the pacemaker spike including the type of pacemaker, such as endocardial, epicardial or leadless; the mode of pacing, such as bipolar versus unipolar pacing; the pacing voltage, and other patient factors which may decrease the overall ECG signal including obesity, emphysema and anasarca [7].
References
- Dalia T, Amr BS. Pacemaker Indications. [Updated 2023 Aug 14]. In: StatPearls [Internet.
- Mulyala A, Parks A, Shah N, Rahman MU, Riad M, Awan GM, Malozzi C, Omar B. Right-Sided Defibrillator: Elevated Defibrillation Threshold! Cardiofel Newslet 2022. Dec; 5(12):36 – 38.
- Lichtenstein BJ, Bichell DP, Connolly DM, Lamberti JJ, Shepard SM, Seslar SP. Surgical approaches to epicardial pacemaker placement: does pocket location affect lead survival? Pediatr Cardiol. 2010 Oct;31(7):1016-24.
- Vouliotis AI, Roberts PR, Dilaveris P, Gatzoulis K, Yue A, Tsioufis K. Leadless Pacemakers: Current Achievements and Future Perspectives. Eur Cardiol. 2023 Aug 18;18:e49.
- Safavi-Naeini P, Saeed M. Pacemaker Troubleshooting: Common Clinical Scenarios. Tex Heart Inst J. 2016 Oct 1;43(5):415-418.
- Andersson HB, Hansen MB, Thorsberger M, Biering-Sørensen T, Nielsen JB, Graff C, Pehrson S, Svendsen JH. Diagnostic accuracy of pace spikes in the electrocardiogram to diagnose paced rhythm. J Electrocardiol. 2015 Sep-Oct;48(5):834-9.
- Madias JE. Decrease/disappearance of pacemaker stimulus "spikes" due to anasarca: further proof that the mechanism of attenuation of ECG voltage with anasarca is extracardiac in origin. Ann Noninvasive Electrocardiol. 2004 Jul;9(3):243-5.
Authors:
Brent Ruiz, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Celestine Odigwe, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hajira Malik, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sanchitha Nagaraj, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mohammad As Sayaideh, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Alexis Parks, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Suganya Manoharan, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Brent Ruiz, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mariam Riad, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Celestine Odigwe, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Hajira Malik, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Sanchitha Nagaraj, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mohammad As Sayaideh, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Alexis Parks, D.O.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Suganya Manoharan, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL