September 2020 Issue
ISSN 2689-291X
ISSN 2689-291X
ECG Findings You Do Not Want To Miss!
Introduction
The electrocardiogram (ECG) remains the cornerstone for the diagnosis of many cardiac conditions [1]. While the ECG report usually provides a description of the recorded electrical findings, ECG interpretation requires a deeper analysis of such findings in relation to a patient’s presentation [2]. The busy clinical schedules of many physicians have resulted in excess reliance on computer ECG interpretations, which may contain inaccuracies and require over-reading by an experienced electrocardiographer [3]. Improving ECG interpretation skills should be a priority in training [4], with application of competency-based approach at both the undergraduate and postgraduate levels [5].
Here, we present three ECGs with questions to illustrate the differential diagnosis and the potential pitfalls of computer interpretations. The reader may choose to systematically interpret the ECG tracings and entertain potential diagnoses [6].
The electrocardiogram (ECG) remains the cornerstone for the diagnosis of many cardiac conditions [1]. While the ECG report usually provides a description of the recorded electrical findings, ECG interpretation requires a deeper analysis of such findings in relation to a patient’s presentation [2]. The busy clinical schedules of many physicians have resulted in excess reliance on computer ECG interpretations, which may contain inaccuracies and require over-reading by an experienced electrocardiographer [3]. Improving ECG interpretation skills should be a priority in training [4], with application of competency-based approach at both the undergraduate and postgraduate levels [5].
Here, we present three ECGs with questions to illustrate the differential diagnosis and the potential pitfalls of computer interpretations. The reader may choose to systematically interpret the ECG tracings and entertain potential diagnoses [6].
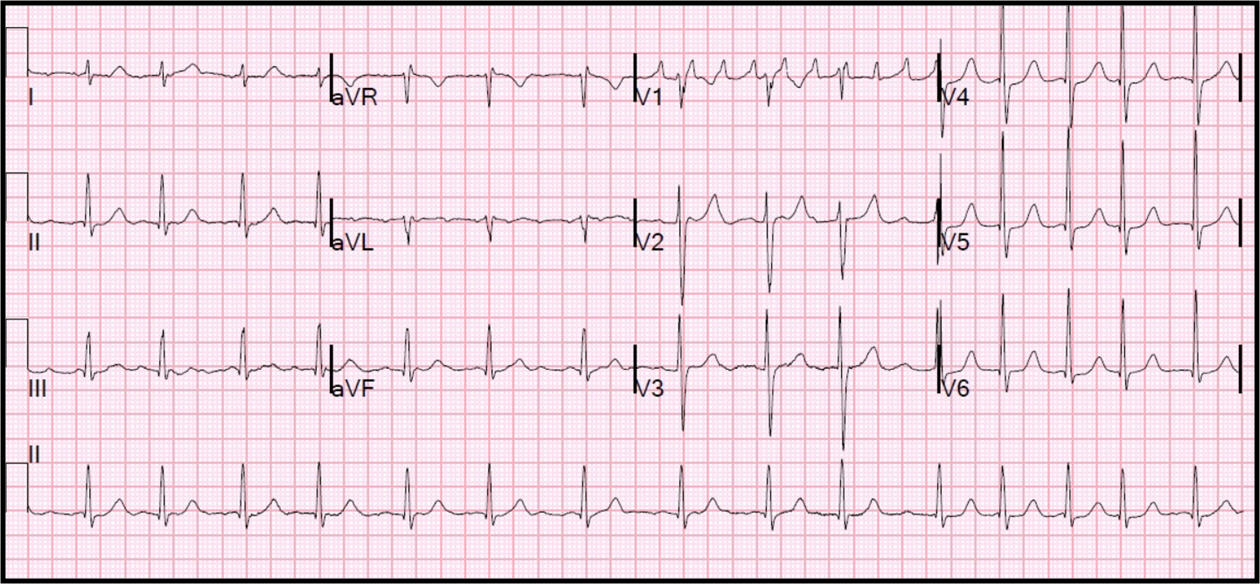
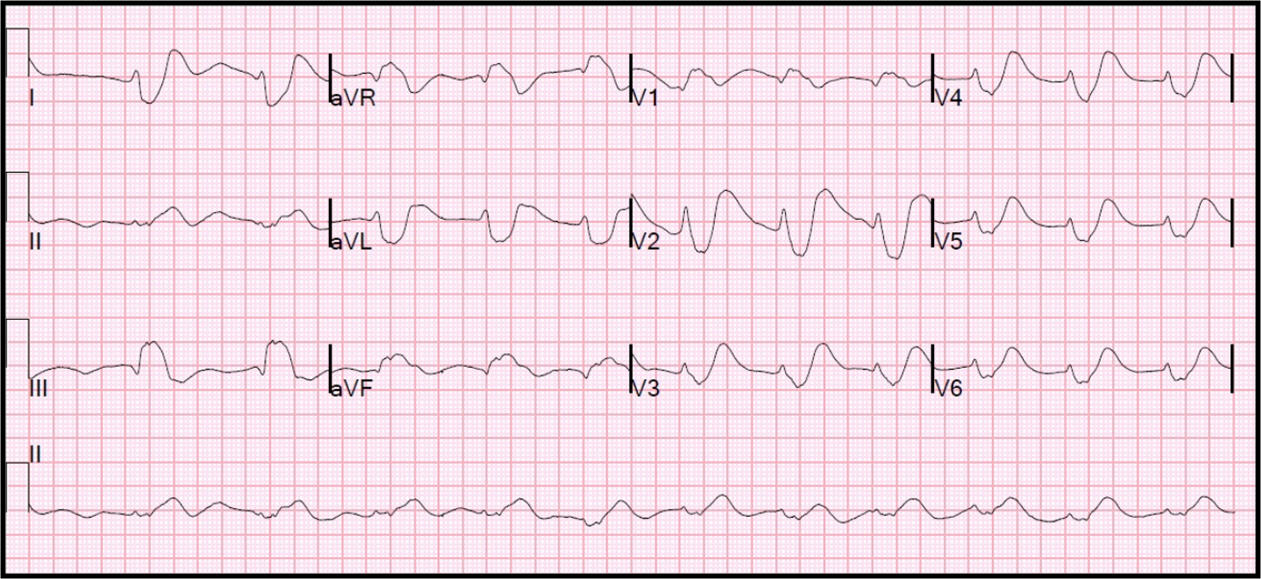
Figure 1A. What is the cause of the irregular rhythm?
A. Sinus rhythm with sinus arrhythmia.
B. Sinus rhythm with intraventricular conduction delay.
C. Atrial flutter with variable AV conduction.
D. Atrial fibrillation with rapid ventricular response.
Discussion:
A. Sinus rhythm with sinus arrhythmia.
B. Sinus rhythm with intraventricular conduction delay.
C. Atrial flutter with variable AV conduction.
D. Atrial fibrillation with rapid ventricular response.
Discussion:
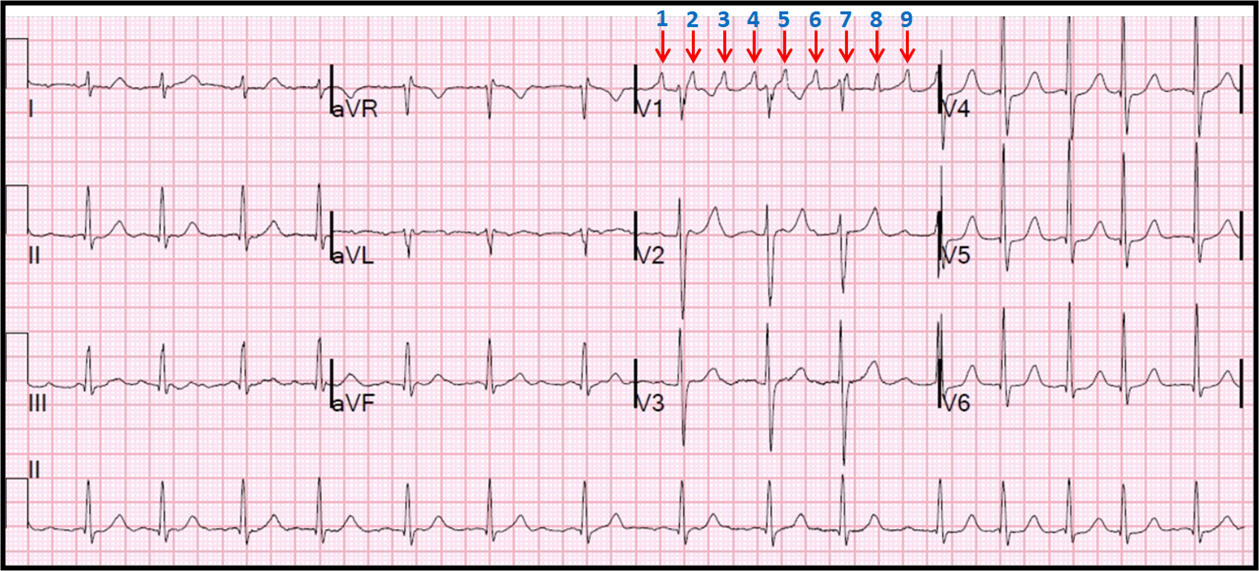
Figure 1B. Atrial flutter with variable AV conduction.
Examining the atrial activity, it is obvious that there are multiple P waves, or F (flutter) waves, seen best in lead V1, with an atrial rate of approximately 240/minute. Looking at Lead II rhythm strip, the irregularity and the inconspicuous P waves may cause a machine reading atrial fibrillation. The 1st and the 4th flutter waves, when viewed in Lead II rhythm strip, may also be misleading as sinus rhythm with sinus arrhythmia. Flutter waves which are adherent to the QRS complex (2nd and 7th) may form a pseudo r’, with an erroneous interpretation of an intraventricular conduction delay. The absence of the typical saw tooth appearance in the inferior leads is suggestive of atypical atrial flutter [7].
Examining the atrial activity, it is obvious that there are multiple P waves, or F (flutter) waves, seen best in lead V1, with an atrial rate of approximately 240/minute. Looking at Lead II rhythm strip, the irregularity and the inconspicuous P waves may cause a machine reading atrial fibrillation. The 1st and the 4th flutter waves, when viewed in Lead II rhythm strip, may also be misleading as sinus rhythm with sinus arrhythmia. Flutter waves which are adherent to the QRS complex (2nd and 7th) may form a pseudo r’, with an erroneous interpretation of an intraventricular conduction delay. The absence of the typical saw tooth appearance in the inferior leads is suggestive of atypical atrial flutter [7].
Figure 2A. What is the cause of abnormalities on this ECG?
A. Old inferior myocardial infarction.
B. Left-sided accessory pathway.
C. Precordial lead misplacement.
D. Right ventricular hypertrophy.
Discussion:
A. Old inferior myocardial infarction.
B. Left-sided accessory pathway.
C. Precordial lead misplacement.
D. Right ventricular hypertrophy.
Discussion:
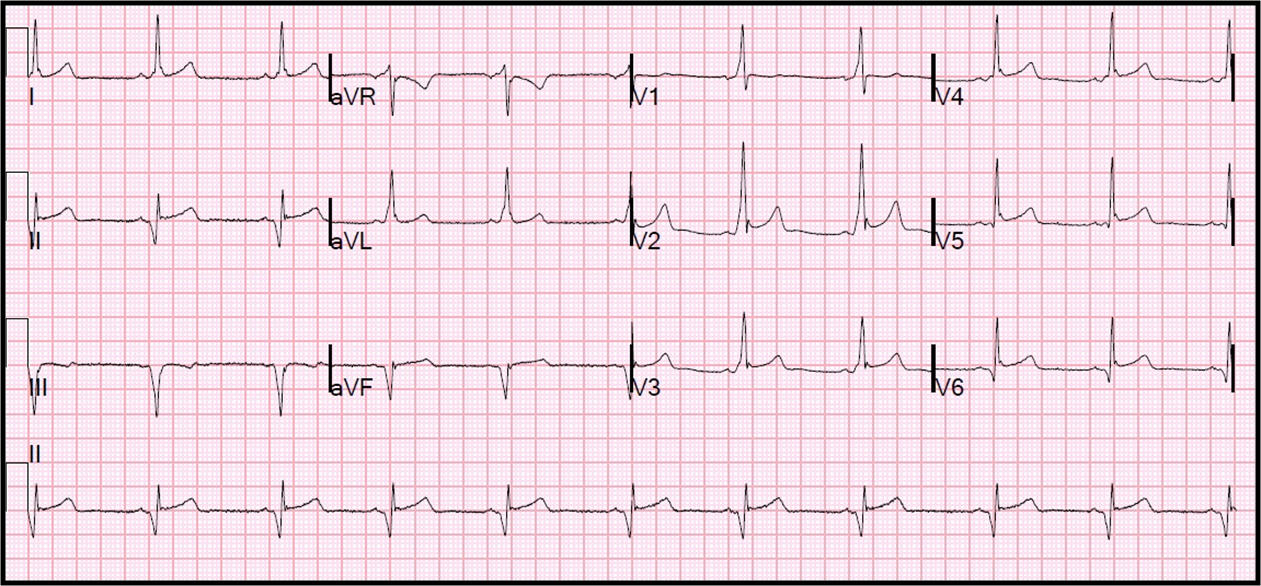
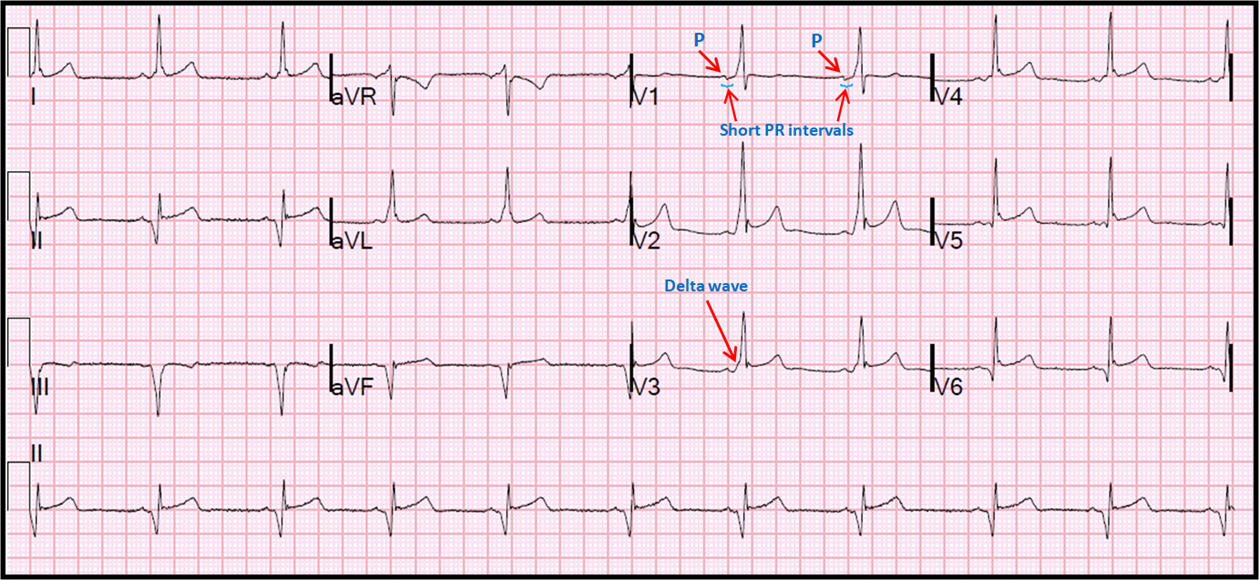
Figure 2B. Left-sided accessory pathway.
The underlying rhythm in this EKG tracing is normal sinus rhythm. There is early transition of the QRS complexes in V1, which may be confused for right ventricular hypertrophy. Q waves in the inferior leads may also lead to an erroneous diagnosis of old inferior myocardial infarction. The precordial lead voltage is positive and concordant, not indicative of lead misplacement. Closer examination reveals a short PR interval and slurring of the initial portion of the QRS complexes due to delta waves. This is typical of left-sided, likely posteroseptal, accessory pathway. The inferior Q waves represent a pseudo-infarct pattern due to altered ventricular activation, a common finding in posteroseptal accessory pathways [8].
The underlying rhythm in this EKG tracing is normal sinus rhythm. There is early transition of the QRS complexes in V1, which may be confused for right ventricular hypertrophy. Q waves in the inferior leads may also lead to an erroneous diagnosis of old inferior myocardial infarction. The precordial lead voltage is positive and concordant, not indicative of lead misplacement. Closer examination reveals a short PR interval and slurring of the initial portion of the QRS complexes due to delta waves. This is typical of left-sided, likely posteroseptal, accessory pathway. The inferior Q waves represent a pseudo-infarct pattern due to altered ventricular activation, a common finding in posteroseptal accessory pathways [8].
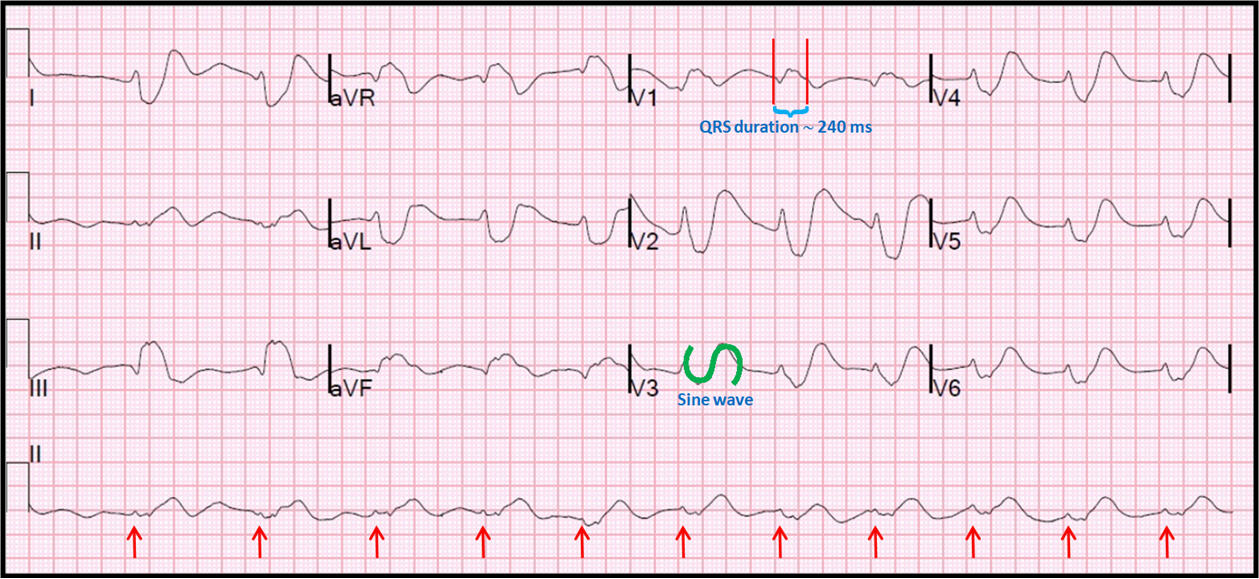
Figure 3A. What is the cause of the bizarre QRS complexes?
A. Hypothermia.
B. Left bundle branch block (LBBB).
C. Anterior ST elevation MI (STEMI).
D. Electrolyte abnormality.
Discussion:
A. Hypothermia.
B. Left bundle branch block (LBBB).
C. Anterior ST elevation MI (STEMI).
D. Electrolyte abnormality.
Discussion:
Figure 3B. Electrolyte abnormality (severe hyperkalemia; potassium level > 10 mmol/L).
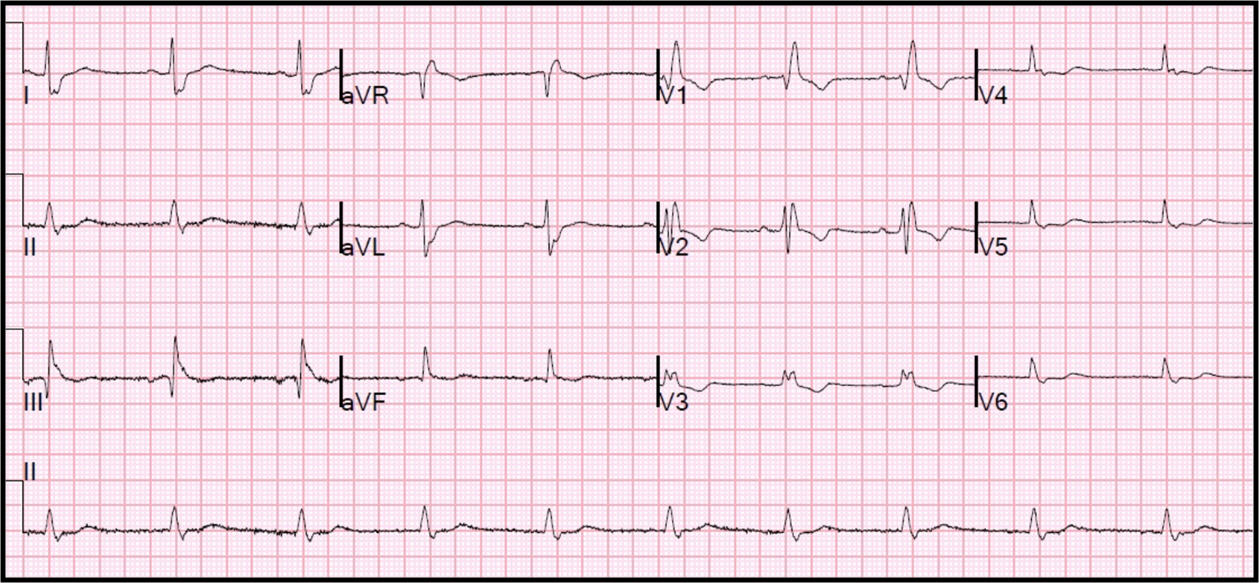
The QRS complexes in this tracing are very wide, unlikely from isolated LBBB. Hypothermia is associated with a terminal positive deflection of the QRS complex, the Osborne (J) wave, not seen here. The QRS widening is causing the QRS to fuse with the T wave, obliterating the ST segment, which is not suggestive of an anterior STEMI. This QRS-T fusion is pathognomonic of
the sine wave of severe hyperkalemia [9]. The underlying rhythm is suggestive of sinus arrhythmia but without conspicuous P waves. This may be due to sinoventricular conduction with loss of atrial capture seen in severe hyperkalemia [10]. Resolution of these changes and return of sinus rhythm is seen on repeat ECG with K ~ 4 (Figure 4).
The QRS complexes in this tracing are very wide, unlikely from isolated LBBB. Hypothermia is associated with a terminal positive deflection of the QRS complex, the Osborne (J) wave, not seen here. The QRS widening is causing the QRS to fuse with the T wave, obliterating the ST segment, which is not suggestive of an anterior STEMI. This QRS-T fusion is pathognomonic of
the sine wave of severe hyperkalemia [9]. The underlying rhythm is suggestive of sinus arrhythmia but without conspicuous P waves. This may be due to sinoventricular conduction with loss of atrial capture seen in severe hyperkalemia [10]. Resolution of these changes and return of sinus rhythm is seen on repeat ECG with K ~ 4 (Figure 4).
Figure 4. Normalization of ECG changes of severe hyperkalemia shown in figure 3.
References:
Authors:
Keerthana Karumbaiah, M.D.
Staff Cardiologist
Shannon Clinic
San Angelo, TX
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulikkumar Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
References:
- Noble RJ, Hillis JS, Rothbaum DA. Electrocardiography. In: Walker HK, Hall WD, Hurst JW, eds. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston: Butterworths; 1990.
- Hurst JW. There is more in the ECG than is reported. Am J Med. 2005;118(12):1453.
- Schläpfer J, Wellens HJ. Computer-Interpreted Electrocardiograms: Benefits and Limitations. J Am Coll Cardiol. 2017;70(9):1183-1192.
- Hurst JW. Current status of clinical electrocardiography with suggestions for the improvement of the interpretive process. Am J Cardiol. 2003;92(9):1072-1079.
- Antiperovitch P, Zareba W, Steinberg JS, et al. Proposed In-Training Electrocardiogram Interpretation Competencies for Undergraduate and Postgraduate Trainees. J Hosp Med.
- Hutton D. A novel systematic approach to ECG interpretation. Dynamics. 2005;16(4): 19-21.
- Cosío FG. Atrial Flutter, Typical and Atypical: A Review. Arrhythm Electrophysiol Rev. 2017;6(2):55-62.
- Goldberger AL. Pseudo-infarct patterns in the Wolff-Parkinson-White syndrome: importance of Q wave-T wave vector discordance. J Electrocardiol. 1980;13(2):115-118.
- Petrov DB. Images in clinical medicine. An electrocardiographic sine wave in hyperkalemia [published correction appears in N Engl J Med. 2012 Nov 8;367(19):1868]. N Engl J Med. 2012;366(19):1824.
- Maradey J, Bhave P. Sinoventricular Conduction in the Setting of Severe Hyperkalemia. JACC Clin Electrophysiol. 2018;4(5):701-70.
Authors:
Keerthana Karumbaiah, M.D.
Staff Cardiologist
Shannon Clinic
San Angelo, TX
Muhammad Rafique, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulikkumar Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
G. Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Beta Blocker Overdose..
Atrial Standstill Then Double Wenckebach!
Introduction
Beta adrenergic receptor blocking agents (beta blockers) are a heterogeneous group of medications with variable physiologic and pharmacologic characteristics making them suitable for use as antihypertensive [1], anti-ischemic [2], antiarrhythmic [3] and heart failure [4] therapies. Certain beta blockers also have more specific noncardiac indications such as in the treatment of hyperthyroidism [5], prevention of migraine headaches [6] and prevention of variceal bleeding in cirrhotic patients [7]. Their ubiquitous use dictates that health care providers should be familiar with the recognition and treatment of beta blocker overdose and toxicity [8].
Beta adrenergic receptor blocking agents (beta blockers) are a heterogeneous group of medications with variable physiologic and pharmacologic characteristics making them suitable for use as antihypertensive [1], anti-ischemic [2], antiarrhythmic [3] and heart failure [4] therapies. Certain beta blockers also have more specific noncardiac indications such as in the treatment of hyperthyroidism [5], prevention of migraine headaches [6] and prevention of variceal bleeding in cirrhotic patients [7]. Their ubiquitous use dictates that health care providers should be familiar with the recognition and treatment of beta blocker overdose and toxicity [8].
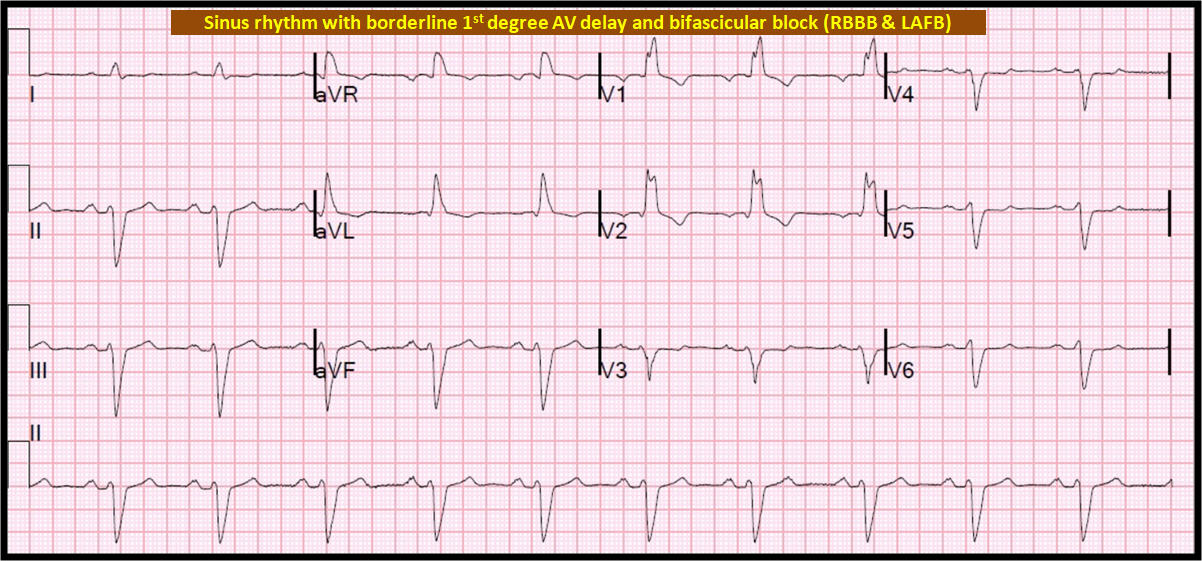
Figure 1. Sinus rhythm 1st degree AV delay and bifascicular block
The above ECG reveals sinus rhythm at 63 beats per minute (BPM). There is borderline first degree AV delay with a PR interval of 210 milliseconds (ms). There is right bundle branch block (RBBB). There is left axis deviation of about – 80 degrees indicative of left anterior
fascicular block. This baseline ECG is indicative of extensive disease in the conduction system often referred to as trifascicular block [9], though this may be a misnomer given that the AV node is not considered a fascicle.
The above ECG reveals sinus rhythm at 63 beats per minute (BPM). There is borderline first degree AV delay with a PR interval of 210 milliseconds (ms). There is right bundle branch block (RBBB). There is left axis deviation of about – 80 degrees indicative of left anterior
fascicular block. This baseline ECG is indicative of extensive disease in the conduction system often referred to as trifascicular block [9], though this may be a misnomer given that the AV node is not considered a fascicle.
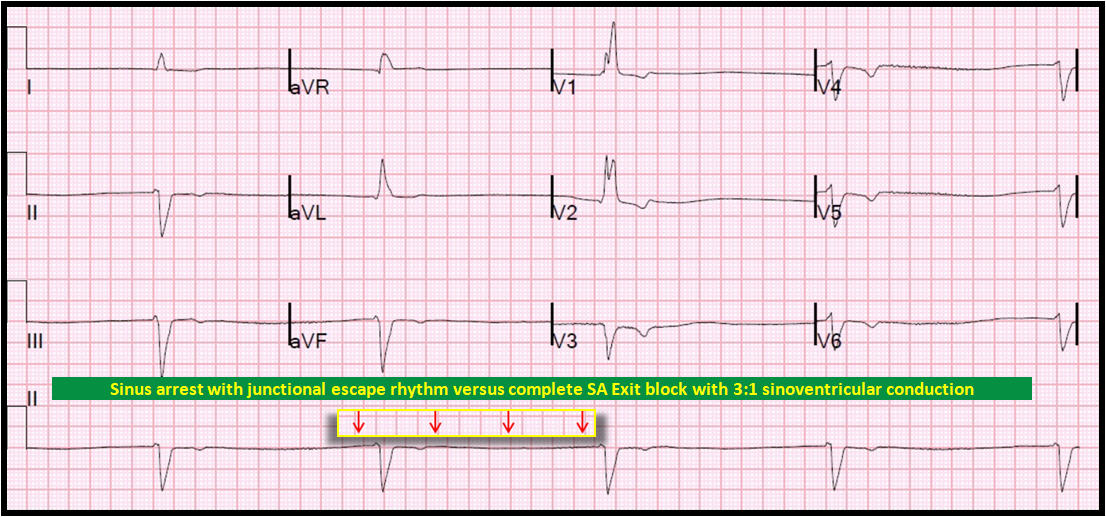
Figure 2. Atrial standstill with wide complex escape rhythm on high dose beta blocker.
The above ECG is the effect of high dose beta blocker on the baseline ECG in Figure 1. There are no P waves (atrial standstill) which may be due to sinus arrest versus complete (third degree) sinoatrial (SA) exit block [10]. The underlying ventricular rhythm is most likely junctional versus sinus capture as is resembles the QRS morphology in Figure 1. The insert represents the simulated sinus rate from Figure 3 to illustrate the possibility of sinus rhythm with complete SA exit block and 3:1 sinoventricular capture [11].
The above ECG is the effect of high dose beta blocker on the baseline ECG in Figure 1. There are no P waves (atrial standstill) which may be due to sinus arrest versus complete (third degree) sinoatrial (SA) exit block [10]. The underlying ventricular rhythm is most likely junctional versus sinus capture as is resembles the QRS morphology in Figure 1. The insert represents the simulated sinus rate from Figure 3 to illustrate the possibility of sinus rhythm with complete SA exit block and 3:1 sinoventricular capture [11].
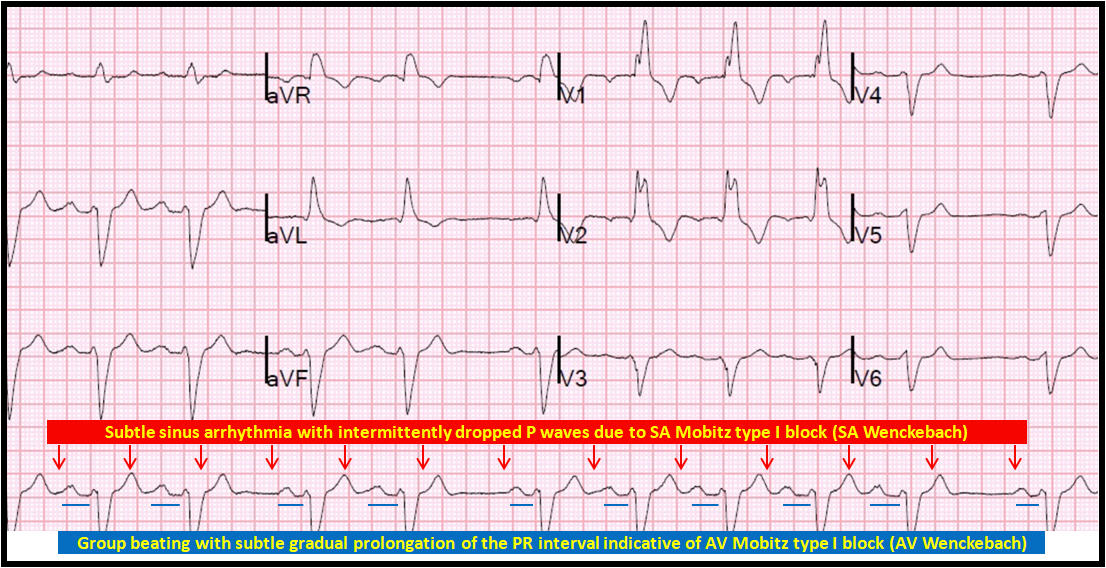
Figure 3. Recovery phase after withdrawal of beta blocker.
The above ECG demonstrates sinus rhythm with borderline first degree AV block, gradual prolongation of the PR interval and group beating suggestive of Mobitz type I AV block (AV Wenckebach). However, there are no blocked P waves when expected. This is often caused by a similar phenomenon at the level of the SA node, with gradual prolongation of the SA conduction until one does not conduct resulting in a pause on the surface ECG; this is second degree type I SA exit block (SA Wenckebach). The simulated sinus rhythm has minor irregularity due to presumed sinus arrhythmia. The R – R intervals in Figure 2 are equivalent to three simulated sinus intervals from Figure 3, therefore suggesting complete SA exit block with 3:1 sinoventricular conduction as the mechanism of the atrial standstill.
References:
Authors:
Keerthana Karumbaiah, M.D.
Staff Cardiologist
Shannon Clinic
San Angelo, TX
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
The above ECG demonstrates sinus rhythm with borderline first degree AV block, gradual prolongation of the PR interval and group beating suggestive of Mobitz type I AV block (AV Wenckebach). However, there are no blocked P waves when expected. This is often caused by a similar phenomenon at the level of the SA node, with gradual prolongation of the SA conduction until one does not conduct resulting in a pause on the surface ECG; this is second degree type I SA exit block (SA Wenckebach). The simulated sinus rhythm has minor irregularity due to presumed sinus arrhythmia. The R – R intervals in Figure 2 are equivalent to three simulated sinus intervals from Figure 3, therefore suggesting complete SA exit block with 3:1 sinoventricular conduction as the mechanism of the atrial standstill.
References:
- Ripley TL, Saseen JJ. β-blockers: a review of their pharmacological and physiological diversity in hypertension. Ann Pharmacother. 2014;48(6):723-733.
- Ablad B, Abrahamsson T, Adler G, et al. Cardiac anti-ischemic effect of metoprolol: role of beta-blockade within the ischemic region. J Cardiovasc Pharmacol. 1987;10 Suppl 2:S117-S127.
- Zicha S, Tsuji Y, Shiroshita-Takeshita A, Nattel S. Beta-blockers as antiarrhythmic agents. Handb Exp Pharmacol. 2006;(171):235-266.
- Klapholz M. Beta-blocker use for the stages of heart failure. Mayo Clin Proc. 2009;84(8):718-729.
- Geffner DL, Hershman JM. Beta-adrenergic blockade for the treatment of hyperthyroidism. Am J Med. 1992;93(1):61-68.
- Jackson JL, Kuriyama A, Kuwatsuka Y, et al. Beta-blockers for the prevention of headache in adults, a systematic review and meta-analysis. PLoS One. 2019;14(3):e0212785.
- Groszmann RJ, Garcia-Tsao G, Bosch J, et al. Beta-blockers to prevent gastroesophageal varices in patients with cirrhosis. N Engl J Med. 2005;353(21):2254-2261.
- Love JN. Beta-blocker toxicity: a clinical diagnosis. Am J Emerg Med. 1994;12(3):356-357.
- Shetty RK, Agarwal S, Ganiga Sanjeeva NC, Rao MS. Trifascicular block progressing to complete AV block on exercise: a rare presentation demonstrating the usefulness of exercise testing. BMJ Case Rep. 2015;2015:bcr2014209180.
- Manne JRR. A case of atenolol-induced sinus node dysfunction presenting as escape-capture bigeminy. Oxf Med Case Reports. 2018;2018(5):omy015.
- Sherf L, James TN. A new electrocardiographic concept: synchronized sinoventricular conduction. Dis Chest. 1969;55(2):127-140.
Authors:
Keerthana Karumbaiah, M.D.
Staff Cardiologist
Shannon Clinic
San Angelo, TX
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL