September 2021 Issue
ISSN 2689-291X
ISSN 2689-291X
The MASTER DAPT Trial:
A Month-DAPT DES!
Abstract
The balance between thrombosis and bleeding risks remains a major consideration driving decisions regarding percutaneous coronary interventions [1]. The MASTER DAPT trial (MAnagement of high bleeding risk patients post bioresorbable polymer coated STEnt implantation with an abbreviated versus prolonged DAPT Regimen) recently published on August 28th, 2021 in the New England Journal of Medicine [2] examined the feasibility of shorter duration dual antiplatelets (DAPT) following a drug-eluting stent (DES) in patients deemed to have a high bleeding risk (HBR). The study details and clinical implications will be reviewed in this paper.
Study Details
- Design: Interventional, randomized, parallel.
- Sites: 140 in 30 countries, excluding USA.
- Subjects: 4579 randomized.
- Started 04/04/2017; completed 04/30/2021
Inclusion criteria:
After index PCI, patients ≥ 18 years are eligible if the following criteria are met:
- ≥ 1 HBR criterion met.
- All lesions successfully treated with Ultimaster stent (<20% residual stenosis).
- No dissection or side-branch occlusion requiring prolonged DAPT.
- All PCI stages complete.
- ≥ 1 HBR criterion or post-PCI actionable non-access site bleeding episode.
- Stable at 30 days: no MI, restenosis, stent thrombosis, stroke or revascularization requiring prolonged DAPT.
- If not on oral anticoagulant (OAC):
a. On aspirin and a P2Y12 inhibitor(i).
b. No P2Y12i switching in previous 7 days. - If on OAC:
a. On same OAC (VKA, NOAC) for ³ 7 days.
b. On clopidogrel for at least 7 days.
- Indication for OAC for ³ 12 months.
- Recent (<12 months) non-access site actionable bleeding.
- Previous bleed requiring hospitalization, if cause has not been definitively treated.
- Age ³ 75 years.
- History or current platelets <100k/mm3, or coagulation disorder with HBR.
- Anemia: hemoglobin <11 g/dl or transfusion within 4 weeks before randomization.
- Need for chronic steroids or NSAIDs.
- Malignancy (other than skin) w/ HBR (including GI, GU/renal & pulmonary).
- Stroke any time or TIA in previous 6 months.
- PRECISE DAPT score ³ 25 [3].
Exclusion criteria:
- PCI with other than Ultimaster stent within 6 months prior to index PCI.
- Rx for instent restenosis or thrombosis at or within 6 months of index PCI.
- PCI with a bioresorbable scaffold at any time prior to index procedure.
- Any planned and anticipated PCI.
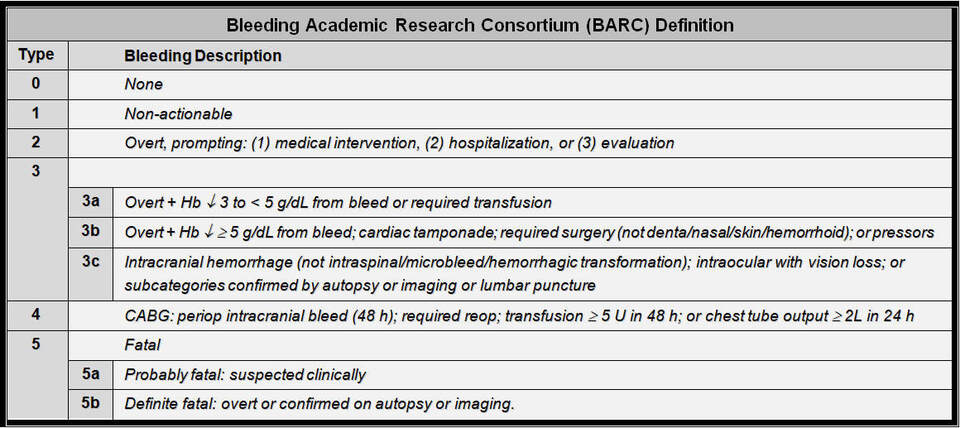
- Active bleed requiring medical attention (BARC ≥ 2; table 1) [4] on randomization visit.
- Allergy to aspirin, clopidogrel, ticagrelor, prasugrel, cobalt chromium or sirolimus.
- Pregnant or breast feeding women
- Life expectancy less than one year. Participation in another trial.
- Cannot consent or comply with protocols. In court protection, tutorship or curatorship.
Treatment Strategies
Randomization 1 month post stent placement:
- Abbreviated DAPT:
- Single antiplatelet ³ 11 months.
- On OAC: ASA or Clopidogrel x 5 months.
- Prolonged DAPT:
- DAPT 5 - 11 months, ASA ³ 11 months.
- On OAC: ASA & Clopidogrel 2 - 11 months.
Results
Primary outcomes: at 335 days
- Net adverse clinical events (NACE) - all-cause death, MI, stroke & bleeding (BARC 3 or 5):
- 7.5% in abbreviated & 7.7% in prolonged DAPT (p < 0.001 for noninferiority).
- Major adverse cardiac/cerebral events (MACCE) - all-cause death, MI & stroke:
- 6.1% in abbreviated & 5.9% in prolonged DAPT (p = 0.001 for noninferiority).
- Major or clinically relevant non-major bleed (MCB) - type 2, 3 and 5 BARC bleeding:
- 6.5% in abbreviated & 9.4% in prolonged DAPT (p < 0.001 for superiority).
Secondary outcomes: at 14 months
- All-cause mortality, MI and stent thrombosis: similar in abbreviated & prolonged DAPT.
- Cerebrovascular events (CVA): 0.8% in abbreviated & 1.4% in prolonged DAPT:
a. Stroke: 0.5% in abbreviated & 1.0% in prolonged DAPT.
b. Hemorrhagic CVA: 1 patient in abbreviated & 5 patients in prolonged DAPT. - BARC type 2 bleeding: 4.5% in abbreviated & 6.8% in prolonged DAPT.
- BARC type 3, 4, or 5 bleeding: 2.3% in abbreviated & 2.6% in prolonged DAPT.
- Fatal bleeding (BARC type 5): 0.1% in abbreviated & 0.4% in prolonged DAPT.
Discussion
The MASTER DAPT trial demonstrated that in HBR patients who received a biodegradable-polymer sirolimus DES, stopping DAPT one month following PCI was noninferior to a longer DAPT regimen with regards to the primary endpoints of NACE and MACCE, and was superior with regards to MCB, seemingly due to lower clinically relevant nonmajor bleeding (BARC 2). Primary outcomes appeared consistent among subgroups. Secondary outcomes were mostly similar in the two groups.
The authors discussed several potential limitations to the study, including the limited enrollment of 4% of screened patients (22% of eligible patients), the open label nature of the study, the exclusion of instent restenosis/stent thrombosis, the variable duration of DAPT in the prolonged treatment group, the different monotherapy used following DAPT in the abbreviated DAPT group, the longer than recommended DAPT in patients on OAC, and the lower than expected NACE & MACCE, with wide noninferiority margins, potentially causing higher event rates with abbreviated DAPT. They also noted that their findings may not necessarily be applicable to non-HBR patients or those who receive a different stent than used in this trial.
Several of those concerns were echoed in an editorial following the publication [5]. This
editorial also commented on the importance of the trial findings in promoting shorter post PCI antithrombotic regimen, especially in the context of chronic disease and high bleeding risk.
Clinical Implications
The science of coronary interventions continues to expand rapidly ever since it started more than 40 years ago [6]. Stent deployment was a major breakthrough in endovascular therapeutics, with drug delivery technology which greatly minimizes the risk of instent restenosis [7]. This, however, has introduced the novel risk of stent thrombosis, mandating prolonged antiplatelet therapy for at least 6 months following drug-eluting stent deployment in the setting of stable coronary disease and 12 months following an acute coronary syndrome, as per the 2016 ACC/AHA guidelines recommendations [8].
A recent large network meta-analysis of dual antiplatelet use following drug eluting stents [9] reasserted the concept that while shorter durations of DAPT followed by P2Y12i monotherapy decreased bleeding risk, extended DAPT use reduced the risk of myocardial infarction while increasing the bleeding risk. To mitigate the increased risk of bleeding in the elderly (³ 75 years), the SENIOR trial [10] reported better outcomes with one months of DAPT following a synergy DES compared with a bare metal stent.
While the risk of bleeding from DAPT has been the subject of several clinical trials and scoring systems, there has been fewer studies and risk scoring schemes which examined the risk of early stent thrombosis [11]. Several studies have addressed the risk of late stent thrombosis and the need for extending DAPT beyond one year [12, 13, 14]. The concept of “tailored” antiplatelet therapy following stent deployment is attractive and will need further development and research, given the heterogeneous patient profiles, clinical presentations and interventional outcomes, making a uniform one-size-fits-all approach inadequate [15]. There remain a few knowledge gaps and unmet needs in DAPT’s optimal regimen, which calls for further research to help individualize its use for safer outcomes.
References
- Mehta SR. Balancing thrombotic events and bleeding in primary PCI. N Engl J Med. 2013 Dec 5;369(23):2263-5.
- Valgimigli M, Frigoli E, Heg D, et al; MASTER DAPT Investigators. Dual Antiplatelet Therapy after PCI in Patients at High Bleeding Risk. N Engl J Med. 2021 Oct 28;385(18):1643-1655.
- Costa F, van Klaveren D, James S, et al; PRECISE-DAPT Study Investigators. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. 2017 Mar 11;389(10073):1025-1034.
- Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011 Jun 14;123(23):2736-47.
- Ohman EM. The Evolving Post-PCI Antithrombotic Therapies. N Engl J Med. 2021 Oct 28;385(18):1712-1714.
- Sachdev S, Tahir H, Awan GM, Omar B. Angioplasty Beginnings..40 Years Later. Cardiofel Newslet 2018 September;1(3):17-18.
- Costa MA, Simon DI. Molecular basis of restenosis and drug-eluting stents. Circulation. 2005 May 3;111(17):2257-73.
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016 Sep 6;68(10):1082-115.
- Khan SU, Singh M, Valavoor S, et al. Dual Antiplatelet Therapy After Percutaneous Coronary Intervention and Drug-Eluting Stents: A Systematic Review and Network Meta-Analysis. Circulation. 2020 Oct 13;142(15):1425-1436.
- Varenne O, Cook S, Sideris G, et al; SENIOR investigators. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. Lancet. 2018 Jan 6;391(10115):41-50.
- Dangas GD, Claessen BE, Mehran R, et al. Development and validation of a stent thrombosis risk score in patients with acute coronary syndromes. JACC Cardiovasc Interv. 2012 Nov;5(11):1097-105.
- Wang X, Chen X, Tian T, You H, et al. A scoring system to predict the occurrence of very late stent thrombosis following percutaneous coronary intervention for acute coronary syndrome. Sci Rep. 2020 Apr 14;10(1):6378.
- Godschalk TC, Gimbel ME, Nolet WW, et al. A clinical risk score to identify patients at high risk of very late stent thrombosis. J Interv Cardiol. 2018 Apr;31(2):159-169.
- Mauri L, Kereiakes DJ, Yeh RW, et al; DAPT Study Investigators. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014 Dec 4;371(23):2155-66.
- van der Sangen NMR, Rozemeijer R, Chan Pin Yin DRPP, et al. Patient-tailored antithrombotic therapy following percutaneous coronary intervention. Eur Heart J. 2021 Mar 7;42(10):1038-1046.
Table 1: Bleeding Academic Research Consortium (BARC) Definition [4]
Authors:
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulik Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Usman Sarwar, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nupur Shah, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Nilarun Chowdhuri, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Maulik Patel, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Siva Chiranjeevi, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Farnoosh Rahimi, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Amod Amritphale, M.D.
Assistant Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Mustafa Awan, M.D.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL