September 2022 Issue
ISSN 2689-291X
ISSN 2689-291X
Sinoatrial Nodal Reentry:
Abrupt Sinus Tachycardia!
Description
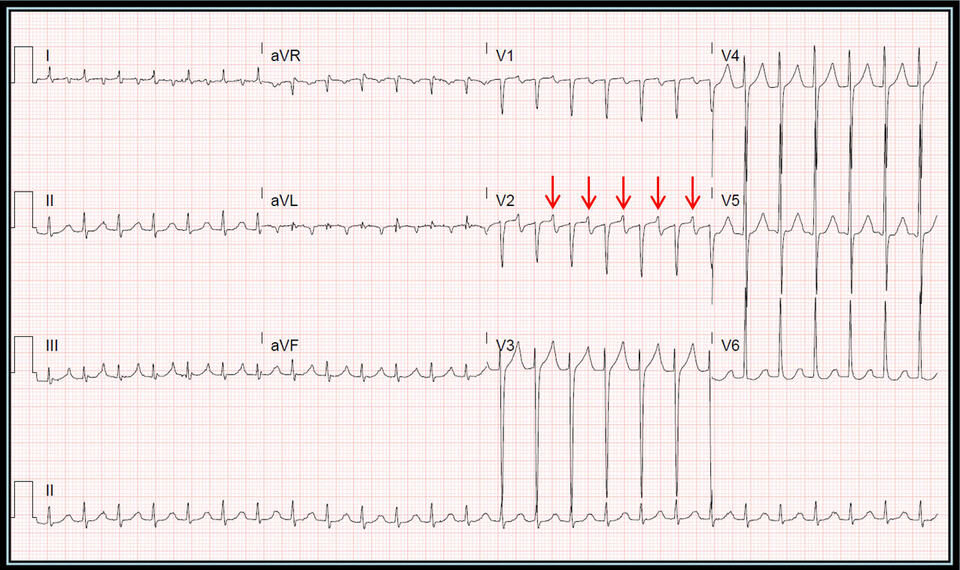
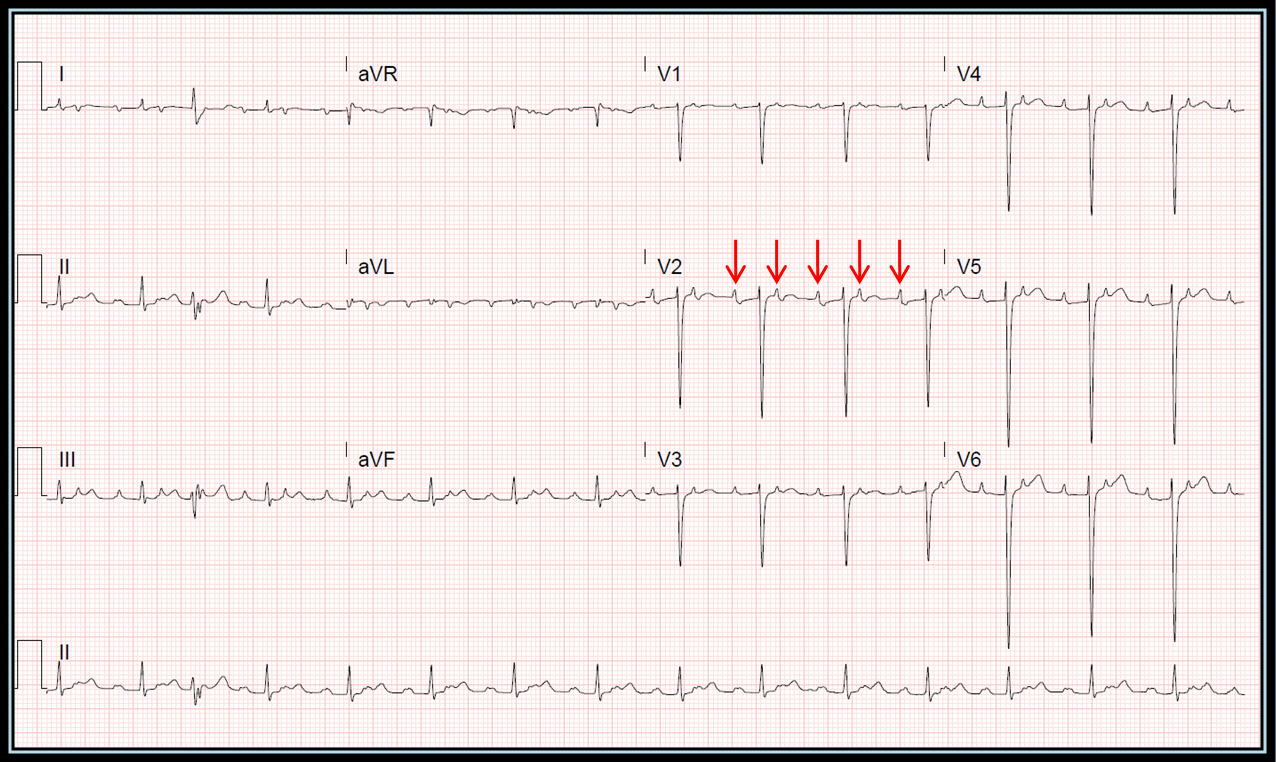
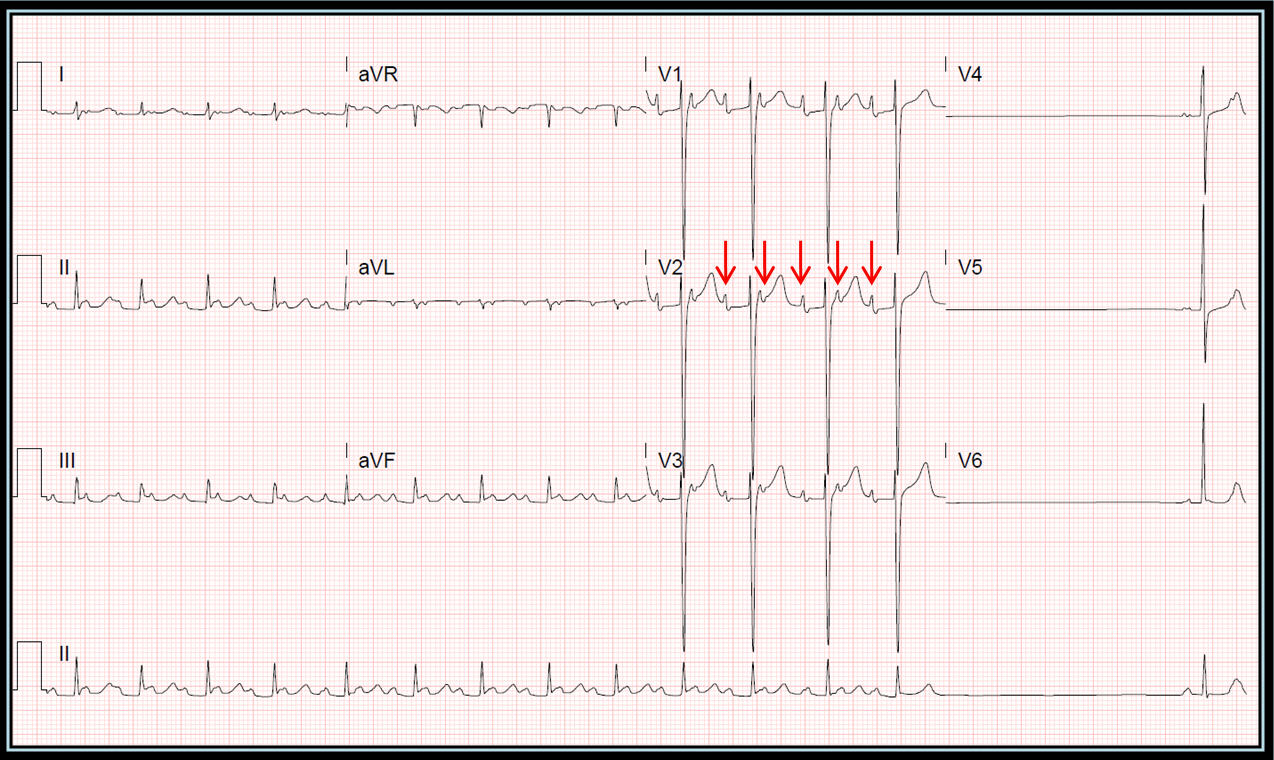
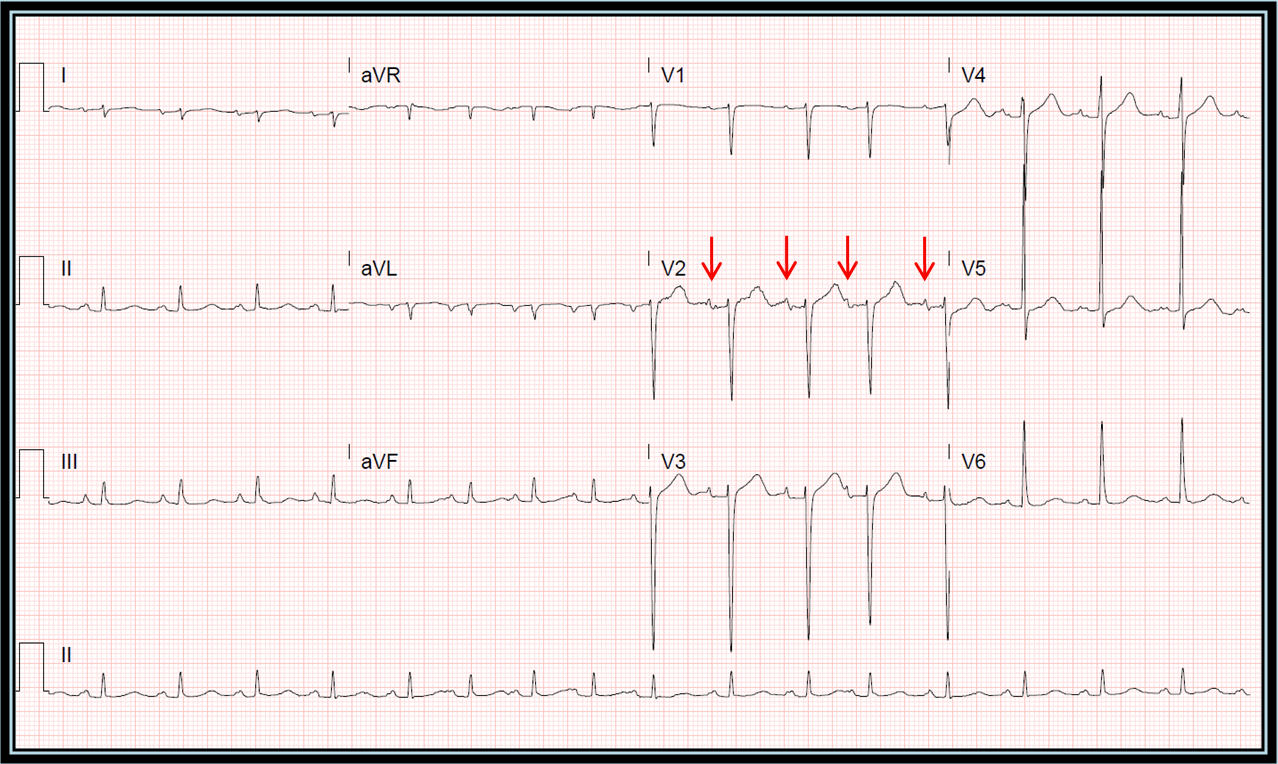
The following series of EKGs are from a patient being treated for respiratory failure. Abrupt sinus tachycardia at 155 beats per minute (BPM) developed as seen in figure 1. Attempts at slowing down the rate with intravenous (IV) metoprolol resulted in development of 2:1 conduction with a ventricular rate of 86 BPM, as seen in figure 2, indicating that the rhythm is unlikely to be sinus rhythm, and likely a form of atrial tachycardia with P wave morphology indicative of sinus origin, suggesting sinoatrial nodal reentry tachycardia (SANRT). Further IV metoprolol resulted in termination of the tachycardia with an initial pause (figure 3), followed by sinus tachycardia at 101 BPM (figure 4) with sinus P waves similar in morphology to the P waves seen during the initial tachycardia, confirming SANRT. The pause seen in figure 3 was likely caused by overdrive suppression of the sinus node by the SANRT. The arrhythmia was successfully suppressed with oral long acting diltiazem.
The following series of EKGs are from a patient being treated for respiratory failure. Abrupt sinus tachycardia at 155 beats per minute (BPM) developed as seen in figure 1. Attempts at slowing down the rate with intravenous (IV) metoprolol resulted in development of 2:1 conduction with a ventricular rate of 86 BPM, as seen in figure 2, indicating that the rhythm is unlikely to be sinus rhythm, and likely a form of atrial tachycardia with P wave morphology indicative of sinus origin, suggesting sinoatrial nodal reentry tachycardia (SANRT). Further IV metoprolol resulted in termination of the tachycardia with an initial pause (figure 3), followed by sinus tachycardia at 101 BPM (figure 4) with sinus P waves similar in morphology to the P waves seen during the initial tachycardia, confirming SANRT. The pause seen in figure 3 was likely caused by overdrive suppression of the sinus node by the SANRT. The arrhythmia was successfully suppressed with oral long acting diltiazem.
Figure 1. Abrupt extreme narrow complex tachycardia with features suggestive of sinus origin (red arrows) and left atrial enlargement.
Figure 2. Following IV metoprolol, atrial rhythm persists (red arrows), but with 2:1 conduction, suggestive of atrial tachycardia of sinus origin (SANRT).
Figure 3: Following further IV metoprolol, the atrial tachycardia breaks with a pause preceding sinus rhythm; suggesting reentry mechanism. Sinus P wave morphology is similar to the atrial tachycardia.
Figure 4: Sinus rhythm resumes following administration of IV metoprolol, with adequate suppression of the tachycardia on oral long-acting diltiazem.
Discussion
Sinoatrial nodal reentrant tachycardia (SANRT) is a rare form of focal tachycardia, caused by reentry circuits originating from or around the sinus node, with abrupt onset and termination, and P wave morphology similar to that of sinus rhythm [1].
Management of symptomatic SANRT can be either pharmacologic with drugs or with ablation [2]. SANRT was reported in approximately 3.2% of patients undergoing electrophysiology (EP) studies for supraventricular tachycardia (SVT) most of whom had successful catheter radiofrequency ablation of the arrhythmia [3].
SANRT was reported in about 17% of EP studies performed for SVT in another study [4]; it was associated with organic heart disease, demonstrated variable cycle length and was shown to be responsive to amiodarone, digoxin and verapamil.
References
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Taylor Goulding-Avedisian, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Phillip Friedlander, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL
Sinoatrial nodal reentrant tachycardia (SANRT) is a rare form of focal tachycardia, caused by reentry circuits originating from or around the sinus node, with abrupt onset and termination, and P wave morphology similar to that of sinus rhythm [1].
Management of symptomatic SANRT can be either pharmacologic with drugs or with ablation [2]. SANRT was reported in approximately 3.2% of patients undergoing electrophysiology (EP) studies for supraventricular tachycardia (SVT) most of whom had successful catheter radiofrequency ablation of the arrhythmia [3].
SANRT was reported in about 17% of EP studies performed for SVT in another study [4]; it was associated with organic heart disease, demonstrated variable cycle length and was shown to be responsive to amiodarone, digoxin and verapamil.
References
- Hafeez Y, Grossman SA. Sinoatrial Nodal Reentrant Tachycardia. 2022 Jul 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–.
- Gomes JA, Mehta D, Langan MN. Sinus node reentrant tachycardia. Pacing Clin Electrophysiol. 1995 May;18(5 Pt 1):1045-57.
- Sanders WE Jr, Sorrentino RA, Greenfield RA, Shenasa H, Hamer ME, Wharton JM. Catheter ablation of sinoatrial node reentrant tachycardia. J Am Coll Cardiol. 1994 Mar 15;23(4):926-34.
- Gomes JA, Hariman RJ, Kang PS, Chowdry IH. Sustained symptomatic sinus node reentrant tachycardia: incidence, clinical significance, electrophysiologic observations and the effects of antiarrhythmic agents. J Am Coll Cardiol. 1985 Jan;5(1):45-57.
Authors:
Rajasekhar Mulyala, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Taylor Goulding-Avedisian, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Phillip Friedlander, M.D.
Internal Medicine Resident
University of South Alabama
Mobile, AL
Nikky Bardia, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Mustafeez Ur Rahman, M.D.
Cardiology Fellow
University of South Alabama
Mobile, AL
Christopher Malozzi, D.O.
Associate Professor of Cardiology
University of South Alabama
Mobile, AL
Bassam Omar, M.D., Ph.D.
Professor of Cardiology
University of South Alabama
Mobile, AL